Chronic Pelvic Pain
Condition Basics
What is chronic pelvic pain?
Pelvic pain is pain below the belly button. It's chronic if you've had pain for at least 6 months. It may be a mild ache that comes and goes. Or you might have a steady, severe pain that makes it hard to sleep, work, or enjoy life.
What causes it?
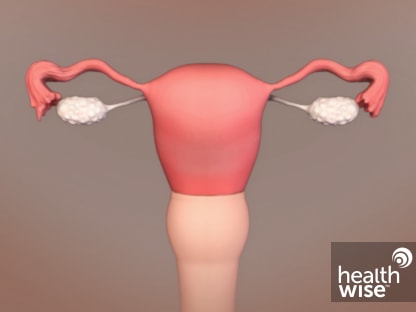
Chronic pelvic pain may be caused by problems in the female reproductive system. These include endometriosis, adenomyosis, and uterine fibroids. Other causes include scar tissue in the pelvic area after an infection or surgery, urinary or bowel diseases, and problems with the muscles, joints, and ligaments in the pelvis, lower back, or hips.
What are the symptoms?
Chronic pelvic pain may include severe cramping during periods, pain during sex, or pain when you urinate or have a bowel movement. You may have pain in certain postures or positions. Pain may range from mild to severe or dull to sharp.
How is it diagnosed?
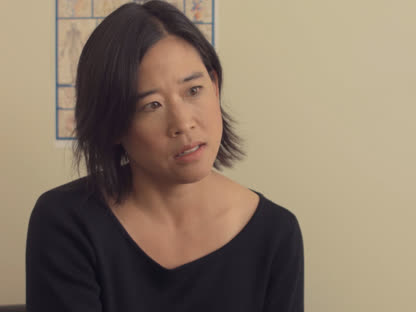
Your doctor may do a pelvic exam to check for problems with your reproductive system. The doctor will ask about your health and symptoms. You may be asked if you have depression or a history of sexual abuse. You may have tests, such as blood and urine tests to check for infection.
How is chronic pelvic pain treated?
Treatment for chronic pelvic pain depends on the cause. Common treatments include birth control pills or hormone treatment for problems related to your periods, or surgery to remove a growth, cyst, or tumor. Or you may get medicine to relieve pain or to help treat the problem that's causing the pain.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
Some common causes of chronic pelvic pain include:
- Problems of the female reproductive system, such as:
- Scar tissue (adhesions) in the pelvic area after an infection or surgery.
- Diseases of the urinary tract or bowel, such as:
- Irritable bowel syndrome.
- Chronic bladder irritation.
- Problems with the muscles, joints, and ligaments in the pelvis, lower back, or hips.
Doctors don't really understand all the things that can cause chronic pelvic pain. So sometimes, even with a lot of testing, the cause remains unknown. This doesn't mean that there isn't a cause or that your pain isn't real.
Sometimes, after a disease has been treated or an injury has healed, the affected nerves keep sending pain signals. This is called neuropathic pain. It may help explain why it can be so hard to find the cause of chronic pelvic pain.
What Increases Your Risk
Risk factors are things that increase your chances of getting a certain condition or disease. Risk factors for pelvic pain that becomes chronic include:
- A history of pelvic inflammatory disease.
- A history of physical or sexual abuse. People with chronic pelvic pain are more likely to report abuse in their past.footnote 1
- A history of radiation treatment or surgery of the abdomen or pelvis. This includes some surgeries for urinary incontinence.
- A history of depression. Pain and depression seem to be related.
- Substance use disorder.
- A problem with the structure of the organs.
- Pregnancy and childbirth that put stress on the back and pelvis. Examples include having a large baby, a difficult delivery, or a forceps or vacuum delivery.
Symptoms
Chronic pelvic pain may include:
- Severe cramping during periods.
- Heavy or irregular vaginal bleeding.
- Pain during sex.
- Pain when you urinate or have a bowel movement.
- Pain in certain postures or positions.
The pain can range from mild to severe or from dull to sharp.
Chronic pain can make it hard to sleep, work, or enjoy life. It can lead to depression. Depression can cause you to feel sad or hopeless, eat and sleep poorly, and move slowly.
Learn more
What Happens
It can sometimes be hard to know how long pelvic pain will last and how best to treat it. It's a little different for everyone. But in general:
- When a cause is found and treated, such as an ovarian cyst, the pain will most likely go away.
- When it's hard to find a cause, your doctor can do a number of tests and try certain treatments to see if they work.
- Symptoms that are caused by hormone fluctuations often go away without treatment when menopause occurs.
- If your pelvic pain is caused by neuropathic pain, your doctor may try certain treatments. Sometimes with neuropathic pain, your nerves still send pain signals long after an injury or disease has healed.
- If your pelvic pain isn't getting better after treatment, you may be referred to a pain management clinic for treatment.
When to Call a Doctor
Call a doctor now if you have sudden, severe pelvic pain, with or without vaginal bleeding.
Call a doctor if:
- Your periods have changed from relatively pain-free to painful.
- Pain interferes with your daily activities.
- You start to have pain during intercourse.
- You have painful urination, blood in your urine, or an inability to control the flow of urine.
- You have blood in your stool or a significant, unexplained change in your bowel movements.
- You notice any new pelvic symptoms.
- You haven't yet seen a doctor about your chronic pelvic pain.
Watchful waiting
Watchful waiting is a wait-and-see approach. If you get better on your own, you won't need treatment. If you get worse, you and your doctor will decide what to do next.
During this period, you can keep a daily record of your symptoms and menstrual cycle and any other life events that you consider important. A watchful waiting period may last from a few days to weeks or possibly months.
Check your symptoms
Exams and Tests
Your doctor may do a pelvic exam to check for problems with your reproductive system. The doctor will ask questions about your health and your symptoms. You may have tests, such as:
- Blood and urine tests to look for infection and other problems.
- A pregnancy test.
- Tests for sexually transmitted infections (STIs).
Emotional issues can play a big role in chronic pain. So your doctor may ask questions to find out if depression or stress is adding to your problem. You may be asked about any past or current sexual or physical abuse.
If the first tests don't find a cause, you may have other tests to look at organs in your belly. These may include:
- Transvaginal ultrasound.
- MRI.
- CT scan of the pelvis.
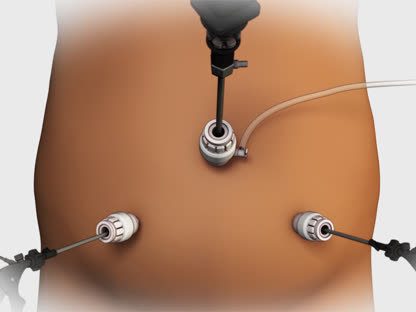
You may also have a type of minor surgery called laparoscopy. This lets the doctor look for problems like growths or scar tissue inside your belly.
Learn more
Watch
Treatment Overview
If your doctor finds a problem that could be causing your pelvic pain, you'll be treated for that problem. Common treatments include:
- Birth control pills or hormone treatment for problems related to your periods.
- Surgery to remove a growth, cyst, or tumor.
- Medicine to treat the problem, such as antibiotics for infection.
Whether or not a cause is found, your doctor can suggest treatments to help manage pain. They include:
- Pain relievers called NSAIDs. These include ibuprofen (such as Advil or Motrin) and naproxen (such as Aleve).
- Antidepressants or anticonvulsants. These can help with pain and with depression.
- Cognitive-behavioral therapy or biofeedback. This may help you change how you think about or react to pain.
- Counseling. It can give you emotional support and reduce stress.
- Physical therapy. It may help you relax your muscles, improve your posture, and be more active.
- Pain relievers that are injected into specific areas to help with pain.
Learn more
Self-Care
You can try these tips at home to ease pelvic pain.
- Try nonprescription medicine.
This includes ibuprofen (such as Advil or Motrin) and acetaminophen (such as Tylenol).
- Try heat.
Put a heating pad, a hot water bottle, or a warm compress on your lower belly, or take a warm bath. Heat improves blood flow and may relieve pain.
- Care for back pain.
Lie down and prop up your legs by placing a pillow under your knees. When lying on your side, bring your knees up to your chest.
- Try relaxation techniques.
These techniques include:
- Meditation.
- Yoga.
- Breathing exercises.
- Progressive muscle relaxation.
- Exercise regularly.
It may help with pain.
Learn more
Watch
Medicines
Medicine won't cure pelvic pain. But it can help control the pain and keep it from getting worse or becoming chronic.
Some medicines help with pain by controlling hormones. They include:
- Hormonal birth control. This may be used for menstrual pain or pain from endometriosis.
- High-dose progestin. It's sometimes prescribed for pain from endometriosis.
- Gonadotropin-releasing hormone agonists. These may help relieve pain from problems such as endometriosis.
Other medicines used for pain include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). They help relieve pain caused by inflammation or menstruation.
- Tricyclic antidepressant medicines. These are sometimes used to treat chronic pain in other areas of the body. They may help relieve chronic pelvic pain in some cases.
- Anticonvulsant medicines, such as gabapentin. They are sometimes used to treat chronic pelvic pain.
Learn more
Watch
Surgery
Surgery for pelvic pain is most likely to help when it's done for a specific condition, like fibroids or endometriosis.
Hysterectomy (removing the uterus) is sometimes done as a last-resort treatment. It may relieve pain in some cases, depending on what caused the pain.
With any surgery for chronic pelvic pain—such as hysterectomy or cutting of specific pelvic-area nerves—there's a risk of lasting pain or pain that's worse after surgery. And it can have serious side effects.
During surgery, the doctor may remove scar tissue (adhesions) from previous surgery or from pelvic inflammatory disease or endometriosis. But most studies have shown that this doesn't relieve pain.footnote 2
Laparoscopy to diagnose chronic pelvic pain may be done before other treatment. Areas of endometriosis or scar tissue may be removed or destroyed during the procedure.
Learn more
Watch
Other Treatment
Counseling-based therapies
Counseling and mental skills training can help when you have chronic pelvic pain. They help you gain the mental and emotional tools to help manage chronic pain and the stress that makes it worse. You can combine medical treatment with other treatments, such as counseling. This can increase your chances of success.
Common treatments include:
- Cognitive-behavioral therapy. It focuses on changing the way you think about and mentally manage pain. A psychologist, licensed counselor, or clinical social worker who specializes in pain management skills can help.
- Biofeedback. This is the conscious control of body function that you normally control unconsciously.
- Interpersonal counseling. It focuses on managing your life events, stressors, and relationships.
Alternative treatments
Alternative pain treatments for chronic pelvic pain aren't well studied. But they may help you to manage stress and learn ways to deal with pain.
Acupuncture and transcutaneous electrical nerve stimulation (TENS) have shown some success in relieving painful menstrual periods. Acupuncture and TENS have also been used as a treatment for nonmenstrual chronic pelvic pain, but this hasn't yet been well studied.footnote 1
There are other low-risk alternative treatments that many people use to help manage pain. They include:
- Relaxation and breathing exercises.
- Hypnosis.
- Guided imagery.
- Aromatherapy.
- Meditation.
- Yoga.
- Massage therapy.
Learn more
Watch
References
Citations
- Andrews J, et al. (2012). Noncyclic Chronic Pelvic Pain Therapies for Women. Comparative Effectiveness Review No. 41 (AHRQ Publication No. 11(12)-EHC088-1). Rockville, MD: Agency for Healthcare Research and Quality. Available online http://www.ncbi.nlm.nih.gov/books/NBK84586.
- Andrews J, et al. (2012). Noncyclic Chronic Pelvic Pain Therapies for Women. Comparative Effectiveness Review No. 41 (AHRQ Publication No. 11(12)-EHC088-1). Rockville, MD: Agency for Healthcare Research and Quality. Available online http://www.ncbi.nlm.nih.gov/books/NBK84586.
Credits
Current as of: April 30, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: April 30, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.