Top of the pageCheck Your Symptoms
Abdominal Pain, Age 11 and Younger
Overview
Abdominal pain, or belly pain, in children is a common problem. But only a small number of these children have a serious problem.
Complaints of belly pain are more common in children younger than 11 years. The pain is often caused by changes in eating and bowel habits. Most cases aren't serious. Home treatment is often all that's needed to help relieve the discomfort.
Belly pain in children can be scary and frustrating for parents. It's often hard to find the exact cause of a child's pain. Pain without other symptoms that goes away completely usually isn't serious.
In children, belly pain may be related to an injury to the abdomen. Or it may be related to an illness, such as a stomach infection, an ear infection, a urinary tract infection, or strep throat. Abdominal symptoms can also occur from an infection passed on by animals or while traveling to a foreign country. Constipation is a common cause of belly pain in children. Some more serious causes in children include appendicitis, lead poisoning, and problems with the intestines, such as intussusception or malrotation. Menstrual periods may cause belly pain each month. The pain may be more severe in some months than others.
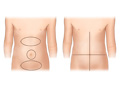
Generalized pain occurs in half of the abdomen or more. Localized pain is located in one area of the abdomen. Babies and toddlers often react differently to pain than older children who can talk about their pain. A baby may be fussy, draw their legs up toward the belly, or eat poorly. Older children may be able to point to the area of the pain and describe how severe it is.
Belly pain can occur one time, or it can occur repeatedly over several months.
Check Your Symptoms
The medical assessment of symptoms is based on the body parts you have.
- If you are transgender or nonbinary, choose the sex that matches the body parts (such as ovaries, testes, prostate, breasts, penis, or vagina) you now have in the area where you are having symptoms.
- If your symptoms aren’t related to those organs, you can choose the gender you identify with.
- If you have some organs of both sexes, you may need to go through this triage tool twice (once as "male" and once as "female"). This will make sure that the tool asks the right questions for you.
Many things can affect how your body responds to a symptom and what kind of care you may need. These include:
- Your age. Babies and older adults tend to get sicker quicker.
- Your overall health. If you have a condition such as diabetes, HIV, cancer, or heart disease, you may need to pay closer attention to certain symptoms and seek care sooner.
- Medicines you take. Certain medicines, such as blood thinners (anticoagulants), medicines that suppress the immune system like steroids or chemotherapy, herbal remedies, or supplements can cause symptoms or make them worse.
- Recent health events, such as surgery or injury. These kinds of events can cause symptoms afterwards or make them more serious.
- Your health habits and lifestyle, such as eating and exercise habits, smoking, alcohol or drug use, sexual history, and travel.
Try Home Treatment
You have answered all the questions. Based on your answers, you may be able to take care of this problem at home.
- Try home treatment to relieve the symptoms.
- Call your doctor if symptoms get worse or you have any concerns (for example, if symptoms are not getting better as you would expect). You may need care sooner.
With cramping pain in the belly:
- The pain may hurt a little or a lot.
- The amount of pain may change from minute to minute. Cramps often get better when you pass gas or have a bowel movement.
- The pain may feel like a tightness or pinching in your belly.
- The pain may be in one specific area or be over a larger area. It may move around.
Babies can quickly get dehydrated when they lose fluids because of problems like vomiting or fever.
Symptoms of dehydration can range from mild to severe. For example:
- The baby may be fussy or cranky (mild dehydration), or the baby may be very sleepy and hard to wake up (severe dehydration).
- The baby may have a little less urine than usual (mild dehydration), or the baby may not be urinating at all (severe dehydration).
You can get dehydrated when you lose a lot of fluids because of problems like vomiting or fever.
Symptoms of dehydration can range from mild to severe. For example:
- You may feel tired and edgy (mild dehydration), or you may feel weak, not alert, and not able to think clearly (severe dehydration).
- You may pass less urine than usual (mild dehydration), or you may not be passing urine at all (severe dehydration).
Severe dehydration means:
- The baby may be very sleepy and hard to wake up.
- The baby may have a very dry mouth and very dry eyes (no tears).
- The baby may have no wet diapers in 12 or more hours.
Moderate dehydration means:
- The baby may have no wet diapers in 6 hours.
- The baby may have a dry mouth and dry eyes (fewer tears than usual).
Mild dehydration means:
- The baby may pass a little less urine than usual.
Severe dehydration means:
- The child's mouth and eyes may be extremely dry.
- The child may pass little or no urine for 12 or more hours.
- The child may not seem alert or able to think clearly.
- The child may be too weak or dizzy to stand.
- The child may pass out.
Moderate dehydration means:
- The child may be a lot more thirsty than usual.
- The child's mouth and eyes may be drier than usual.
- The child may pass little or no urine for 8 or more hours.
- The child may feel dizzy when he or she stands or sits up.
Mild dehydration means:
- The child may be more thirsty than usual.
- The child may pass less urine than usual.
If you're not sure if a child's fever is high, moderate, or mild, think about these issues:
With a high fever:
- The child feels very hot.
- It is likely one of the highest fevers the child has ever had.
With a moderate fever:
- The child feels warm or hot.
- You are sure the child has a fever.
With a mild fever:
- The child may feel a little warm.
- You think the child might have a fever, but you're not sure.
A baby that is extremely sick:
- May be limp and floppy like a rag doll.
- May not respond at all to being held, touched, or talked to.
- May be hard to wake up.
A baby that is sick (but not extremely sick):
- May be sleepier than usual.
- May not eat or drink as much as usual.
Pain in children under 3 years
It can be hard to tell how much pain a baby or toddler is in.
- Severe pain (8 to 10): The pain is so bad that the baby cannot sleep, cannot get comfortable, and cries constantly no matter what you do. The baby may kick, make fists, or grimace.
- Moderate pain (5 to 7): The baby is very fussy, clings to you a lot, and may have trouble sleeping but responds when you try to comfort him or her.
- Mild pain (1 to 4): The baby is a little fussy and clings to you a little but responds when you try to comfort him or her.
Pain in children 3 years and older
- Severe pain (8 to 10): The pain is so bad that the child can't stand it for more than a few hours, can't sleep, and can't do anything else except focus on the pain. No one can tolerate severe pain for more than a few hours.
- Moderate pain (5 to 7): The pain is bad enough to disrupt the child's normal activities and sleep, but the child can tolerate it for hours or days.
- Mild pain (1 to 4): The child notices and may complain of the pain, but it is not bad enough to disrupt his or her sleep or activities.
Shock is a life-threatening condition that may occur quickly after a sudden illness or injury.
Babies and young children often have several symptoms of shock. These include:
- Passing out (losing consciousness).
- Being very sleepy or hard to wake up.
- Not responding when being touched or talked to.
- Breathing much faster than usual.
- Acting confused. The child may not know where he or she is.
Blood in the stool can come from anywhere in the digestive tract, such as the stomach or intestines. Depending on where the blood is coming from and how fast it is moving, it may be bright red, reddish brown, or black like tar.
A little bit of bright red blood on the stool or on the toilet paper is often caused by mild irritation of the rectum. For example, this can happen if you have to strain hard to pass a stool or if you have a hemorrhoid.
A large amount of blood in the stool may mean a more serious problem is present. For example, if there is a lot of blood in the stool, not just on the surface, you may need to call your doctor right away. If there are just a few drops on the stool or in the diaper, you may need to let your doctor know today to discuss your symptoms. Black stools may mean you have blood in the digestive tract that may need treatment right away, or may go away on its own.
Certain medicines and foods can affect the color of stool. Diarrhea medicines (such as Pepto-Bismol) and iron tablets can make the stool black. Eating lots of beets may turn the stool red. Eating foods with black or dark blue food coloring can turn the stool black.
If you take aspirin or some other medicine (called a blood thinner) that prevents blood clots, it can cause some blood in your stools. If you take a blood thinner and have ongoing blood in your stools, call your doctor to discuss your symptoms.
Certain health conditions and medicines weaken the immune system's ability to fight off infection and illness. Some examples in children are:
- Diseases such as diabetes, cystic fibrosis, sickle cell disease, and congenital heart disease.
- Steroid medicines, which are used to treat a variety of conditions.
- Medicines taken after organ transplant.
- Chemotherapy and radiation therapy for cancer.
- Not having a spleen.
Temperature varies a little depending on how you measure it. For children up to 11 years old, here are the ranges for high, moderate, and mild according to how you took the temperature.
Oral (by mouth), ear, or rectal temperature
- High: 104° F (40° C) and higher
- Moderate: 100.4° F (38° C) to 103.9° F (39.9° C)
- Mild: 100.3° F (37.9° C) and lower
A forehead (temporal) scanner is usually 0.5° F (0.3° C) to 1° F (0.6° C) lower than an oral temperature.
Armpit (axillary) temperature
- High: 103° F (39.5° C) and higher
- Moderate: 99.4° F (37.4° C) to 102.9° F (39.4° C)
- Mild: 99.3° F (37.3° C) and lower
Note: For children under 5 years old, rectal temperatures are the most accurate.
It is easy for your diabetes to become out of control when you are sick. Because of an illness:
- Your blood sugar may be too high or too low.
- You may not be able take your diabetes medicine (if you are vomiting or having trouble keeping food or fluids down).
- You may not know how to adjust the timing or dose of your diabetes medicine.
- You may not be eating enough or drinking enough fluids.
An illness plan for people with diabetes usually covers things like:
- How often to test blood sugar and what the target range is.
- Whether and how to adjust the dose and timing of insulin or other diabetes medicines.
- What to do if you have trouble keeping food or fluids down.
- When to call your doctor.
The plan is designed to help keep your diabetes in control even though you are sick. When you have diabetes, even a minor illness can cause problems.
Many prescription and nonprescription medicines can cause belly pain or cramping. A few examples are:
- Aspirin, ibuprofen (such as Advil or Motrin), and naproxen (such as Aleve).
- Antibiotics.
- Antidiarrheals.
- Laxatives.
- Iron supplements.
Seek Care Today
Based on your answers, you may need care soon. The problem probably will not get better without medical care.
- Call your doctor today to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or you don't have one, seek care today.
- If it is evening, watch the symptoms and seek care in the morning.
- If the symptoms get worse, seek care sooner.
Seek Care Now
Based on your answers, you may need care right away. The problem is likely to get worse without medical care.
- Call your doctor now to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or you don't have one, seek care in the next hour.
- You do not need to call an ambulance unless:
- You cannot travel safely either by driving yourself or by having someone else drive you.
- You are in an area where heavy traffic or other problems may slow you down.
Call 911 Now
Based on your answers, you need emergency care.
Call 911 or other emergency services now.
Sometimes people don't want to call 911. They may think that their symptoms aren't serious or that they can just get someone else to drive them. Or they might be concerned about the cost. But based on your answers, the safest and quickest way for you to get the care you need is to call 911 for medical transport to the hospital.
Make an Appointment
Based on your answers, the problem may not improve without medical care.
- Make an appointment to see your doctor in the next 1 to 2 weeks.
- If appropriate, try home treatment while you are waiting for the appointment.
- If symptoms get worse or you have any concerns, call your doctor. You may need care sooner.
Self-Care
Most of the time, a child's abdominal pain, or belly pain, will get better with home treatment. The child won't need a visit to a doctor.
Home treatment for mild belly pain often depends on other symptoms that the child has along with the pain, such as diarrhea, nausea, or vomiting.
Try the following, one at a time in the order listed, if your child has mild belly pain without other symptoms.
- Have your child rest when they have mild belly pain. Most symptoms will get better or go away in 30 minutes.
- Have your child sip clear fluids. Try fluids like water, broth, tea, or fruit juice diluted with water.
- Have your child try to pass a stool.
If the above steps don't work, you may also try these.
- Serve your child several small meals instead of 2 or 3 large ones.
- When your child feels like eating again, start with small amounts. Avoid spicy, hot, or high-fat foods and drinks with caffeine for a day or two. These foods may make your child's belly pain worse.
- Don't give your child any medicines unless you talk to the doctor first. Medicines may mask the pain or make it worse.
Recurrent abdominal pain
A child who has chronic abdominal pain should eat regular meals, not skip any meals, and not overeat at any one meal. Different foods, such as spicy foods or dairy foods, may trigger an episode in some children. Your child should not eat any foods that cause abdominal pain.
Many children are able to manage their pain and keep doing normal activities. Be sure that your child has regular meal and snack times as well as a regular bedtime so your child gets enough sleep.
When to call for help during self-care
Call a doctor if any of the following occur during self-care at home:
- Pain gets worse, does not improve, or is felt in one specific area of the belly.
- Other symptoms develop, such as diarrhea, nausea, vomiting, or a fever.
- The belly feels hard or looks very swollen.
- Symptoms occur more often or are more severe.
Learn more
Preparing For Your Appointment
You can help your doctor diagnose and treat your condition by being prepared for your appointment.
Credits
Current as of: October 19, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: October 19, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.