Childhood Oral Cavity Cancer (PDQ®): Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
What is childhood oral cavity cancer?
Childhood oral cavity cancer is a rare type of cancer that forms in the mouth. There are several types of oral cavity cancers, including lymphoma, sarcoma, squamous cell carcinoma, and mucoepidermoid carcinoma. Most of the tumors (more than 90%) that children get in their mouth are not cancer. All types of tumors in the mouth can affect eating or speaking and need treatment.
The oral cavity includes:
- the front two-thirds of the tongue
- the gums (gingiva)
- the lining of the inside of the cheeks (buccal mucosa)
- the bottom (floor) of the mouth under the tongue
- the roof of the mouth (hard palate)
- the small area behind the wisdom teeth (retromolar trigone)
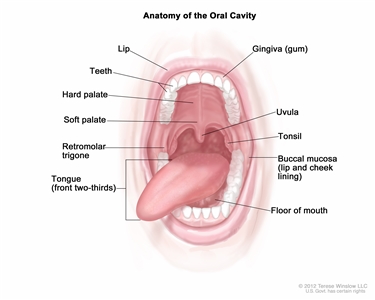
Anatomy of the oral cavity. The oral cavity includes the lips, hard palate (the bony front portion of the roof of the mouth), soft palate (the muscular back portion of the roof of the mouth), retromolar trigone (the area behind the wisdom teeth), front two-thirds of the tongue, gingiva (gums), buccal mucosa (the inner lining of the lips and cheeks), and floor of the mouth under the tongue.
Causes and risk factors for childhood oral cavity cancer
Oral cavity cancer is caused by certain changes to the way the cells in the oral cavity function, especially how they grow and divide into new cells. Often, the exact cause of these cell changes is unknown. Learn more about how cancer develops at What Is Cancer?
A risk factor is anything that increases the chance of getting a disease. Not every child with one or more of these risk factors will develop oral cavity cancer. And it will develop in some children who don't have a known risk factor.
Risk factors for oral cavity cancer in children and adolescents include:
- HPV infection
- having certain genetic conditions, such as:
- Fanconi anemia
- dyskeratosis congenita
- connexin gene mutations
- epidermolysis bullosa
- xeroderma pigmentosum
- having chronic graft-versus-host disease
Getting the HPV vaccine can protect against HPV infection and lower the risk of this and many other types of cancer. Learn more about HPV and Cancer.
Talk with your child's doctor if you think your child may be at risk.
Symptoms of childhood oral cavity cancer
The symptoms of oral cavity cancer may be similar to an infection. It's important to check with your child's doctor if your child has:
- a sore in the mouth that does not heal
- a lump or thickening in the mouth
- a white or red patch on the gums, tongue, or lining of the mouth
- bleeding or pain in the mouth
These symptoms may be caused by problems other than oral cavity cancer. The only way to know is to see your child's doctor.
Tests to diagnose childhood oral cavity cancer
If your child has symptoms that suggest an oral cavity cancer, the doctor will need to find out if these are due to cancer or another problem. The doctor will ask when the symptoms started and how often your child has been having them. They will also ask about your child's personal and family health history and do a physical exam. Depending on these results, they may recommend other tests. If your child is diagnosed with oral cavity cancer, the results of these tests will help you and your child's doctor plan treatment.
The tests used to diagnose oral cavity cancer may include:
Oral exam
In an oral exam, a medical doctor or dentist checks the mouth for abnormal areas. This exam may be done while under anesthesia. The doctor or dentist will feel the entire inside of the mouth with a gloved finger and examine the oral cavity with a small long-handled mirror and lights or a fiberoptic device. This will include checking the insides of the cheeks and lips; the gums; the roof and floor of the mouth; and the top, bottom, and sides of the tongue. The neck will be felt for swollen lymph nodes. A dental exam may also be done.
X-ray
An x-ray is a type of radiation that can go through the body and make pictures of the inside of the body.
Magnetic resonance imaging (MRI)
MRI uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas of the body, such as the head and neck. This procedure is also called nuclear magnetic resonance imaging (NMRI).
Magnetic resonance imaging (MRI) scan. The child lies on a table that slides into the MRI machine, which takes a series of detailed pictures of areas inside the body. The positioning of the child on the table depends on the part of the body being imaged.
CT scan (CAT scan)
A CT scan uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. A dye may be injected into a vein or swallowed to help the tissues or organs show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography. To learn more, see Computed Tomography (CT) Scans and Cancer.
Computed tomography (CT) scan of the head and neck. The child lies on a table that slides through the CT scanner, which takes a series of detailed x-ray pictures of the inside of the head and neck.
PET scan (positron emission tomography scan)
A PET scan uses a small amount of radioactive sugar (also called radioactive glucose) that is injected into the vein. Then a scanner is used to make detailed, computerized pictures of areas inside the body where the glucose is taken up. Because cancer cells often take up more glucose than normal cells, the pictures can be used to find cancer cells in the body.
Positron emission tomography (PET) scan. The child lies on a table that slides through the PET scanner. The head rest and white strap help the child lie still. A small amount of radioactive glucose (sugar) is injected into the child's vein, and a scanner makes a picture of where the glucose is being used in the body. Cancer cells show up brighter in the picture because they take up more glucose than normal cells do.
Biopsy
A biopsy is a procedure in which a sample of tissue is removed from the tumor so that a pathologist can view it under a microscope to check for signs of cancer.
- Fine-needle aspiration biopsy is the removal of cells, tissue or fluid using a thin needle.
- Incisional biopsy is the surgical removal of part of a lump or a sample of tissue that doesn't look normal.
Getting a second opinion
You may want to get a second opinion to confirm your child's cancer diagnosis and treatment plan. If you seek a second opinion, you will need to get medical test results and reports from the first doctor to share with the second doctor. The second doctor will review the pathology report, slides, and scans. This doctor may agree with the first doctor, suggest changes to the treatment plan, or provide more information about your child's cancer.
To learn more about choosing a doctor and getting a second opinion, see Finding Cancer Care. You can contact NCI's Cancer Information Service via chat, email, or phone (both in English and Spanish) for help finding a doctor or hospital that can provide a second opinion. For questions you might want to ask at your child's appointments, see Questions to Ask Your Doctor about Cancer.
Who treats children with oral cavity cancer?
A pediatric oncologist, a doctor who specializes in treating children with cancer, oversees treatment of oral cavity cancer. The pediatric oncologist works with other health care providers who are experts in treating children with cancer and who specialize in certain areas of medicine. Other specialists may include:
- pediatrician
- pediatric surgeon
- radiation oncologist
- pathologist
- ear, nose, and throat specialist
- pediatric nurse specialist
- social worker
- rehabilitation specialist
- psychologist
- child-life specialist
Treatment of childhood oral cavity cancer
There are different types of treatment for children with oral cavity cancer. You and your child's care team will work together to decide treatment. Many factors will be considered, such as where the cancer is located and your child's age and overall health.
Your child's treatment plan will include information about the cancer, the goals of treatment, treatment options, and the possible side effects. It will be helpful to talk with your child's care team before treatment begins about what to expect. For help every step of the way, see our booklet, Children with Cancer: A Guide for Parents.
For oral cavity cancer in children, treatment might include:
- Surgery is the most common treatment for oral cavity cancer in children. For children with an oral cavity tumor that is not cancer, surgery is likely the only treatment that will be needed. Learn more about Surgery to Treat Cancer.
- Chemotherapy (also called chemo) uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. Chemotherapy may be given with other types of treatments.
Chemotherapy can be given in different ways. For oral cavity cancer, chemotherapy is injected into a vein, enabling it to reach cancer cells throughout the body. Learn more about Chemotherapy to Treat Cancer.
- Radiation therapy uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. The type of radiation therapy most often used for oral cavity cancer is external beam radiation therapy. This treatment uses a machine outside the body to send radiation toward the area of the body with cancer. Learn more about External Beam Radiation Therapy for Cancer and Radiation Therapy Side Effects.
Clinical trials
For some children, joining a clinical trial may be an option. There are different types of clinical trials for childhood cancer. For example, a treatment trial tests new treatments or new ways of using current treatments. Supportive care and palliative care trials look at ways to improve quality of life, especially for those who have side effects from cancer and its treatment.
You can use the clinical trial search to find NCI-supported cancer clinical trials accepting participants. The search allows you to filter trials based on the type of cancer, your child's age, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Learn more about clinical trials, including how to find and join one, at Clinical Trials Information for Patients and Caregivers.
Follow-up care
As your child goes through treatment, they will have follow-up tests or check-ups. Some of the tests that were done to diagnose the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your child's condition changes or if the cancer has come back.
Coping with your child's cancer
When your child has cancer, every member of the family needs support. Taking care of yourself during this difficult time is important. Reach out to your child's treatment team and to people in your family and community for support. To learn more, see Support for Families: Childhood Cancer and the booklet Children with Cancer: A Guide for Parents.
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of childhood oral cavity cancer. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Pediatric Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Childhood Oral Cavity Cancer. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/head-and-neck/patient/child/oral-cavity-treatment-pdq. Accessed <MM/DD/YYYY>.
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2024-10-09
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.

