Coronary Angioplasty
Treatment Overview
Coronary angioplasty is a procedure to open a blocked or narrow coronary artery. Coronary arteries are the blood vessels that bring oxygen to the heart muscle. It may also be called percutaneous coronary intervention (PCI).
Angioplasty helps blood flow more normally to the heart muscle. If you have coronary artery disease, it may be done to relieve angina symptoms such as chest pain or pressure. Angioplasty can also be done during or after a heart attack. As a treatment for a heart attack, it may also prevent heart problems.
Before an angioplasty, a doctor does a coronary angiogram. This finds narrowed or blocked arteries. The doctor inserts a thin, flexible tube called a catheter into an artery in your upper leg (groin) or wrist. The doctor moves the catheter through that artery to the coronary arteries. The doctor then uses dye to see any arteries that are blocked or narrowed.
If you have a blocked or narrow artery, a tiny balloon is moved through the catheter. It is used to open the artery. The doctor can also use the balloon to place a stent in the artery to keep it open.
The procedure may take 30 to 90 minutes. But you need time to get ready for it and time to recover. It can take several hours total. You may go home the same day. Or you may stay at least 1 night in the hospital.
How It Is Done
Narrowed or blocked coronary artery
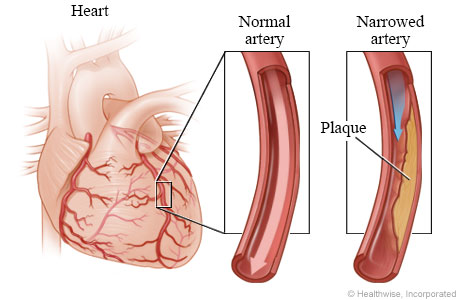
Coronary arteries are the blood vessels that supply oxygen-rich blood to the heart muscle. Coronary artery disease can cause plaque to build up inside the walls of the coronary arteries. Plaque is made up of extra cholesterol, calcium, and other substances that float in blood.
This plaque buildup may narrow the artery and reduce the blood flow to the heart muscle. This narrowing can cause angina symptoms such as chest pain or pressure. Sometimes the plaque can tear or rupture. The body tries to repair the tear by forming a blood clot over it. The blood clot can completely block blood flow and cause a heart attack. A procedure called angioplasty can widen a narrowed or blocked coronary artery.
Step 1: During an angioplasty, a catheter is moved into the coronary artery
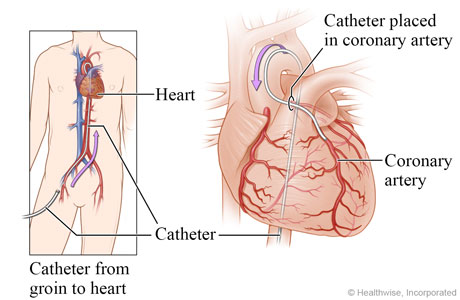
An angioplasty is done using a thin, soft tube called a catheter. The catheter is guided into the blood vessels of the heart. First, your doctor inserts the catheter into a blood vessel in the groin, arm, or wrist. A very thin guide wire is inside the catheter. Your doctor carefully guides the catheter through blood vessels to the narrowed or blocked portion of the coronary artery. Your doctor watches the movement of the catheter in the blood vessels on an X-ray screen.
Step 2: A guide wire and balloon are placed in the coronary artery
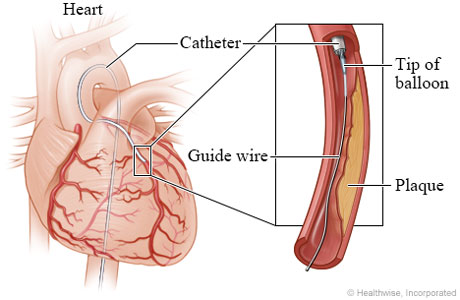
After the catheter reaches the artery, your doctor will move the guide wire farther into the narrowed or blocked portion. A small balloon is slid along the guide wire. In most cases, a small, expandable stent is placed in the artery with the balloon.
Step 3: The balloon is inflated
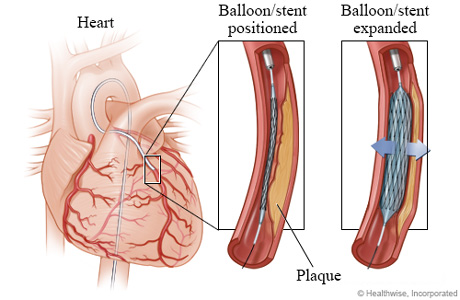
The small balloon is inflated. The balloon may stay inflated for a short time. The pressure from the inflated balloon presses the plaque against the wall of the artery, creating more room for blood to flow. The inflated balloon also expands the stent.
Step 4: The balloon, guide wire, and catheter are removed
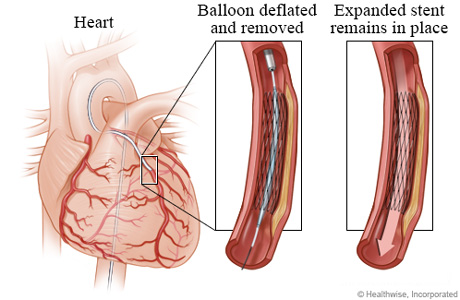
Next, the balloon is deflated. But the stent stays expanded. The stent presses against the walls of the artery and keeps the artery open. Your doctor removes the balloon, guide wire, and catheter. The stent remains in the blood vessel, allowing the blood to flow normally again.
Improved blood flow
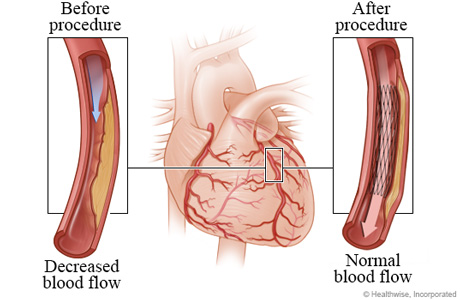
After an angioplasty, the narrowed or blocked artery is opened up and oxygen- and nutrient-rich blood flows more normally into the heart muscle.
Arteries before and after an angioplasty
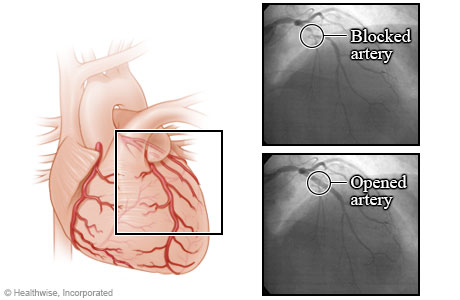
These X-rays show a blocked coronary artery before and after an angioplasty procedure. Before angioplasty, the blood flow is blocked by a narrowed artery. After the angioplasty, blood is flowing better through the newly opened artery. These X-rays are from an angiogram. An angiogram is a test that uses a special dye and camera to take X-ray pictures of the blood flow in an artery.
What To Expect
After a coronary angioplasty, you will be moved to a recovery room or to the coronary care unit. Your heart rate and blood pressure will be closely monitored. The catheter insertion site will be checked for bleeding. You may have a bandage or a compression device on your groin or wrist at the catheter insertion site. This is to prevent bleeding. You may go home the same day. Or you may stay at least 1 night in the hospital.
Do not do strenuous exercise and do not lift anything heavy until your doctor says it is okay. This may be for several days.
You will take medicine to prevent blood clots. This medicine helps prevent a heart attack. If you get a stent, you may take aspirin plus another blood thinner. If you get a drug-eluting stent, you may take both of these medicines for at least 6 months. If you get a bare-metal stent, you may take both medicines for at least 1 month. If you had a heart attack, you may take both medicines for at least 1 year. Then you will likely continue to take one of the medicines. If you have a high risk of bleeding, your doctor may shorten the time you take these medicines. You can work with your doctor to decide how long you will take both of these medicines. This decision may depend on your risk of a heart attack, your risk of bleeding, and your preferences about taking medicine.
After your procedure, you might attend a cardiac rehabilitation (rehab) program. In cardiac rehab, a team of health professionals provides education and support to help you recover and start new, healthy habits, such as eating healthy and getting more exercise. Making these changes is just as important as getting treatment if you want to keep your heart healthy and your arteries open. If your doctor hasn't already suggested it, ask if cardiac rehab is right for you.
Learn more
Watch
Why It Is Done
Coronary angioplasty is done to widen a blocked or narrowed coronary artery and improve blood flow to the heart muscle. It may be done to treat a heart attack or relieve symptoms of stable angina.
Heart attack
Emergency angioplasty may be the first choice of treatment for a heart attack.footnote 1
Doctors try to do angioplasty as soon as possible after a heart attack. But angioplasty is not available in all hospitals. If you are at a hospital that does not do angioplasty, you might be moved to another hospital where angioplasty can be done.
Stable angina
Although many things are involved, angioplasty might be done for stable angina if you:footnote 1
- Have frequent or severe angina that is not responding to medicine and lifestyle changes.
- Had a test that showed severely reduced blood flow (ischemia) to an area of heart muscle caused by one narrowed coronary artery.
- Have an artery that is likely to be treated successfully with angioplasty.
- Are in good enough health to have the procedure.
Angioplasty may not be a reasonable treatment option when:
- There is no evidence of reduced blood flow to the heart muscle.
- You do not have angina symptoms, or you feel that you can live well with your symptoms.
- You are at risk of complications or dying during angioplasty due to other health problems.
- The anatomy of the artery makes angioplasty or stenting too risky or will interfere with the success of the procedure.
How Well It Works
Heart attack
Angioplasty works well to open a blocked artery after a heart attack. This helps blood to flow more normally to the heart muscle. Angioplasty can help lower the risk of death and complications from the heart attack.
Stable angina
Angioplasty can improve your angina symptoms. It can also improve your quality of life. If your symptoms happen a lot, you are more likely to have a better quality of life after the procedure.footnote 2
Angioplasty might not relieve all of your symptoms. But you might not need to take angina medicines anymore. Or you might not need to take as much.
There are some things that angioplasty can't do. In people who have stable angina:footnote 3
- It does not prevent a heart attack.
- It does not help you live longer.
It may be hard to understand why angioplasty does not lower your risk of a heart attack or help you live longer. It's because of how coronary artery disease and plaque happen in your arteries.
Even if you get a stent, you still may have other places in your arteries where a heart attack can happen. During the procedure, your doctor finds and treats the places where plaque narrows the artery and limits blood flow. But smaller plaques can build up in other places in your arteries. They don't limit blood flow much or cause symptoms. But if one ruptures, it can cause a heart attack. This type of plaque is treated with medicines and a heart-healthy lifestyle.
Risks
Angioplasty has some risks. They include:
- The need for emergency bypass surgery during the procedure.
- Heart attack.
- Stroke.
- Death.
Your doctor can help you know your chance of problems. Several things, including age and health, can raise your risk of problems. For example, older people or those with heart failure or kidney disease have a higher risk of problems.
The risks of problems where the catheter was placed include:
- Bleeding.
- Damage to blood vessels.
- Pain.
- Swelling.
- Bruising.
- Tenderness.
Over time, there is a chance that blood vessels with stents can close. There also is a chance that you'll need to decide whether or not to have another angioplasty or a bypass surgery.
Radiation: There is always a slight risk of damage to cells or tissues from being exposed to any radiation. This includes the low levels of X-ray used for this procedure. But the risk of damage from the X-rays is usually very low compared with the possible benefits of the procedure.
References
Citations
- Lawton JS, et al. (2022). 2021 ACC/AHA/SCAI Guideline for coronary artery revascularization: A report from the American College of Cardiology/American Heart Association. Journal of the American College of Cardiology, 79(2): e21–e129. DOI: 10.1016/j.jacc.2021.09.006. Accessed December 9, 2021.
- Spertus JA, et al. (2020). Health-status outcomes with invasive or conservative care in coronary disease. The New England Journal of Medicine, 382(15): 1408–1419. DOI: 10.1056/NEJMoa1916370. Accessed April 2, 2020.
- Bangalore S, et al. (2020). Routine revascularization versus initial medical therapy for stable ischemic heart disease: A systematic review and meta-analysis of randomized trials. Circulation, published online June 26, 2020. DOI: 10.1161/CIRCULATIONAHA.120.048194. Accessed June 26, 2020.
Credits
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.







