Acute Lymphoblastic Leukemia Treatment (PDQ®): Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
General Information About Acute Lymphoblastic Leukemia
Acute lymphoblastic leukemia (ALL) is a type of cancer in which the bone marrow makes too many lymphocytes (a type of white blood cell).
Acute lymphoblastic leukemia (ALL; also called acute lymphocytic leukemia) is a cancer of the blood and bone marrow. This type of cancer usually gets worse quickly if it is not treated.
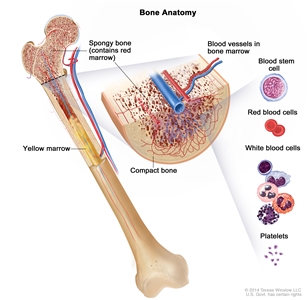
Anatomy of the bone. The bone is made up of compact bone, spongy bone, and bone marrow. Compact bone makes up the outer layer of the bone. Spongy bone is found mostly at the ends of bones and contains red marrow. Bone marrow is found in the center of most bones and has many blood vessels. There are two types of bone marrow: red and yellow. Red marrow contains blood stem cells that can become red blood cells, white blood cells, or platelets. Yellow marrow is made mostly of fat.
Leukemia may affect red blood cells, white blood cells, and platelets.
The bone marrow and thymus make blood stem cells (immature cells) that become mature blood cells over time. A blood stem cell may become a myeloid stem cell or a lymphoid stem cell.
A lymphoid stem cell becomes a lymphoblast cell and then one of three types of lymphocytes (white blood cells):
- B lymphocytes that make antibodies to help fight infection
- T lymphocytes that help B lymphocytes make the antibodies that help fight infection
- natural killer cells that attack cancer cells and viruses
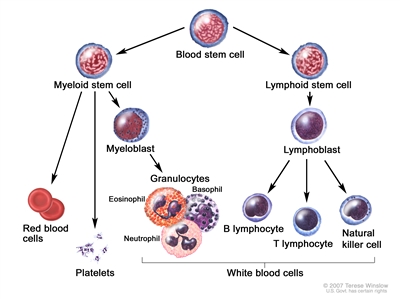
Blood cell development. A blood stem cell goes through several steps to become a red blood cell, platelet, or white blood cell.
In ALL, too many stem cells become lymphoblasts, B lymphocytes, or T lymphocytes. These cells are also called leukemia cells. Leukemia cells are not able to fight infection very well. Also, as the number of leukemia cells increases in the blood and bone marrow, there is less room for healthy white blood cells, red blood cells, and platelets. This may cause infection, anemia, and easy bleeding. The cancer can also spread to the central nervous system (brain and spinal cord), lymph nodes, spleen, liver, testicles, and other organs.
Previous chemotherapy and exposure to radiation may increase the risk of developing ALL.
ALL is caused by certain changes to the way blood stem cells function, especially how they grow and divide into new cells. A risk factor is anything that increases the chance of getting a disease. Some risk factors for cancer, like smoking, can be changed. However, risk factors also include things people cannot change, like their genetics, getting older, and their health history.
There are many risk factors for ALL, but many do not directly cause cancer. Instead, they increase the chance of DNA damage in cells that may lead to ALL. Learn more about how cancer develops at What Is Cancer?
Having one or more of these risk factors does not mean that you will get ALL. Many people with risk factors never develop ALL, while others with no known risk factors do.
Possible risk factors for ALL include:
- being male
- being White
- being older than 70
- past treatment with chemotherapy or radiation therapy
- being exposed to high levels of radiation in the environment (such as nuclear radiation)
- having certain genetic disorders, such as Down syndrome
Talk with your doctor if you think you may be at risk.
Signs and symptoms of ALL include fatigue, fever, and easy bruising or bleeding.
The early signs and symptoms of ALL may be like the flu or other common diseases. Check with your doctor if you have:
- weakness or fatigue
- fever or drenching night sweats
- easy bruising or bleeding
- petechiae (flat, pinpoint spots under the skin, caused by bleeding)
- shortness of breath
- weight loss or loss of appetite
- pain in the bones or stomach
- pain or feeling of fullness below the ribs
- painless lumps in the neck, underarm, stomach, or groin
- frequent infections
These and other signs and symptoms may be caused by ALL or by other conditions.
Tests that examine the blood and bone marrow are used to diagnose ALL.
In addition to asking about your personal and family health history and doing a physical exam, your doctor may perform the following tests and procedures:
- Complete blood count (CBC) with differential is a procedure in which a sample of blood is drawn and checked for:
- the number of red blood cells and platelets
- the number and type of white blood cells
- the amount of hemoglobin (the substance that carries oxygen) in the red blood cells
- the amount of hematocrit (whole blood that is made up of red blood cells)
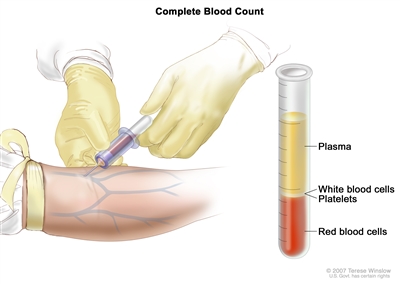
Complete blood count (CBC). Blood is collected by inserting a needle into a vein and allowing the blood to flow into a tube. The blood sample is sent to the laboratory and the red blood cells, white blood cells, and platelets are counted. The CBC is used to test for, diagnose, and monitor many different conditions. - Blood chemistry study is a laboratory test in which a blood sample is checked to measure the amounts of certain substances released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- Peripheral blood smear is a laboratory test in which a sample of blood is checked for blast cells, the number and kinds of white blood cells, the number of platelets, and changes in the shape of blood cells.
- Bone marrow aspiration and biopsy is the removal of bone marrow, blood, and a small piece of bone by inserting a hollow needle into the hipbone or breastbone. A pathologist views the bone marrow, blood, and bone under a microscope to look for abnormal cells.
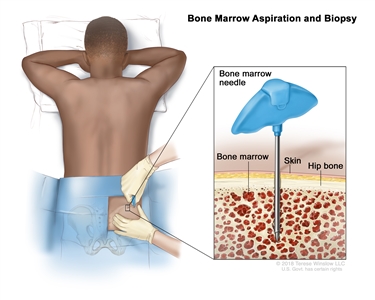
Bone marrow aspiration and biopsy. After a small area of skin is numbed, a long, hollow needle is inserted through the patient's skin and hip bone into the bone marrow. A sample of bone marrow and a small piece of bone are removed for examination under a microscope.The following tests may be done on the samples of blood or bone marrow tissue that are removed:
- Cytogenetic analysis checks the chromosomes of cells in a blood or bone marrow sample for changes, such as broken, missing, rearranged, or extra chromosomes. Changes in certain chromosomes may be a sign of cancer. For example, in Philadelphia chromosome –positive ALL, part of one chromosome switches places with part of another chromosome. This is called the "Philadelphia chromosome." Cytogenetic analysis is used to help diagnose cancer, plan treatment, or find out how well treatment is working.
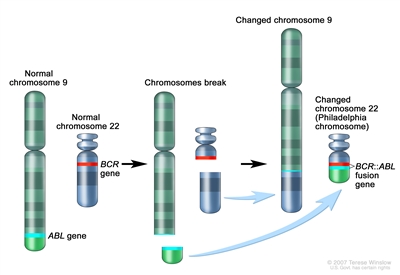
The Philadelphia (Ph) chromosome is an abnormal chromosome that is made when pieces of chromosomes 9 and 22 break off and trade places. The ABL gene from chromosome 9 joins to the BCR gene on chromosome 22 to form the BCR::ABL fusion gene. The changed chromosome 22 with the fusion gene on it is called the Ph chromosome. - Immunophenotyping uses antibodies to identify cancer cells based on the types of antigens or markers on the surface of the cells. This test is used to help diagnose specific types of leukemia. For example, a cytochemistry study may test the cells in a sample of tissue using chemicals (dyes) to look for certain changes in the sample. A chemical may cause a color change in one type of leukemia cell but not in another type of leukemia cell.
- Cytogenetic analysis checks the chromosomes of cells in a blood or bone marrow sample for changes, such as broken, missing, rearranged, or extra chromosomes. Changes in certain chromosomes may be a sign of cancer. For example, in Philadelphia chromosome –positive ALL, part of one chromosome switches places with part of another chromosome. This is called the "Philadelphia chromosome." Cytogenetic analysis is used to help diagnose cancer, plan treatment, or find out how well treatment is working.
After ALL has been diagnosed, tests are done to find out if the cancer has spread to the central nervous system (brain and spinal cord) or to other parts of the body.
The following tests and procedures may be used to find out if the leukemia has spread outside the blood and bone marrow:
- Chest x-ray is a type of radiation that can go through the body and make pictures of the organs and bones inside the chest.
- Lumbar puncture is a procedure used to collect a sample of cerebrospinal fluid (CSF) from the spinal column. This is done by placing a needle between two bones in the spine and into the CSF around the spinal cord and removing a sample of the fluid. The sample of CSF is checked under a microscope for signs that leukemia cells have spread to the brain and spinal cord. This procedure is also called an LP or spinal tap.
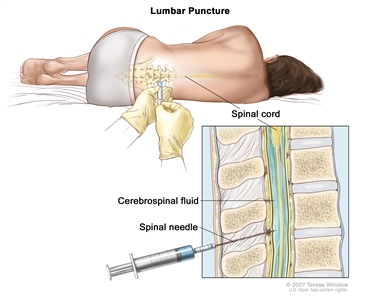
Lumbar puncture. A patient lies in a curled position on a table. After a small area on the lower back is numbed, a spinal needle (a long, thin needle) is inserted into the lower part of the spinal column to remove cerebrospinal fluid (CSF, shown in blue). The fluid may be sent to a laboratory for testing. - CT scan (CAT scan) uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body, such as the abdomen. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- MRI (magnetic resonance imaging) uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
Some people decide to get a second opinion.
You may want to get a second opinion to confirm your ALL diagnosis and treatment plan. If you seek a second opinion, you will need to get medical test results and reports from the first doctor to share with the second doctor. The second doctor will review the pathology report, slides, and scans. They may agree with the first doctor, suggest changes or another treatment approach, or provide more information about your cancer.
To learn more about choosing a doctor and getting a second opinion, see Finding Cancer Care. You can contact NCI's Cancer Information Service via chat, email, or phone (both in English and Spanish) for help finding a doctor, hospital, or getting a second opinion. For questions you might want to ask at your appointments, see Questions to Ask Your Doctor About Cancer.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis and treatment options depend on:
- the person's age
- whether the cancer has spread to the brain or spinal cord
- whether there are certain changes in the genes, including the Philadelphia chromosome
- whether the cancer has been treated before or has recurred (come back)
Stages of Acute Lymphoblastic Leukemia
There is no standard staging system for ALL.
The extent or spread of cancer is usually described as stages. Instead of stages, ALL treatment is based on whether the cancer is untreated, in remission, or recurrent.
Untreated ALL
In untreated ALL, the disease is newly diagnosed. It has not been treated, except to relieve signs and symptoms caused by the cancer, such as fever, bleeding, or pain, and the following are true:
- The complete blood count (CBC) is abnormal.
- More than 5% of the cells in the bone marrow are blasts (leukemia cells).
- There are signs and symptoms of leukemia.
ALL in remission
In ALL in remission, the disease has been treated, and the following are true:
- The CBC is normal.
- 5% or fewer of the cells in the bone marrow are blasts (leukemia cells).
- There are no signs or symptoms of leukemia other than in the bone marrow.
Recurrent ALL
Recurrent ALL is cancer that has recurred (come back) after going into remission. ALL may come back in the blood, bone marrow, or other parts of the body.
Treatment Option Overview
There are different types of treatment for patients with ALL.
Different types of treatment are available for people with ALL. You and your cancer care team will work together to decide your treatment plan, which may include more than one type of treatment. Many factors will be considered, such as whether the ALL is untreated, in remission, or recurrent, and your overall health and preferences. Your plan will include information about your cancer, the goals of treatment, your treatment options and the possible side effects, and the expected length of treatment.
Talking with your cancer care team before treatment begins about what to expect will be helpful. You'll want to learn what you need to do before treatment begins, how you'll feel while going through it, and what kind of help you will need. Learn more at Questions to Ask Your Doctor About Treatment.
The treatment of ALL usually has two phases.
The treatment of ALL is done in phases:
- Remission induction therapy is the first phase of treatment. The goal is to kill the leukemia cells in the blood and bone marrow. This puts the leukemia into remission.
- Post-remission therapy is the second phase of treatment. It begins once the leukemia is in remission. The goal of post-remission therapy is to kill any remaining leukemia cells that may not be active but could begin to regrow and cause a relapse. This phase is also called remission continuation therapy.
Treatment called central nervous system (CNS) prophylaxis is usually given during each phase of therapy. Because standard doses of chemotherapy may not reach leukemia cells in the CNS (brain and spinal cord), the leukemia cells are able to hide in the CNS. Systemic chemotherapy given in high doses, intrathecal chemotherapy, and radiation therapy to the brain are able to reach leukemia cells in the CNS. These treatments are given to kill the leukemia cells and lessen the chance the leukemia will recur (come back).
The following types of treatment are used:
Chemotherapy
Chemotherapy (also called chemo) uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. The way the chemotherapy is given depends on whether the leukemia cells have spread to the central nervous system (CNS; brain and spinal cord).
Systemic chemotherapy is when chemotherapy drugs are taken by mouth or injected into a vein or muscle. When given this way, the drugs enter the bloodstream and can reach cancer cells throughout the body.
Intrathecal chemotherapy may be used to treat ALL that has spread, or may spread, to the brain and spinal cord. Intrathecal chemotherapy is a method of placing chemotherapy directly into the cerebrospinal fluid, which is the fluid that surrounds the brain and spinal cord. When used to lessen the chance leukemia cells will spread to the brain and spinal cord, it is called CNS prophylaxis. 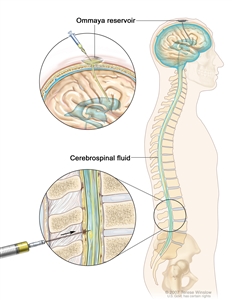
Intrathecal chemotherapy. Anticancer drugs are injected into the intrathecal space, which is the space that holds the cerebrospinal fluid (CSF, shown in blue). There are two different ways to do this. One way, shown in the top part of the figure, is to inject the drugs into an Ommaya reservoir (a dome-shaped container that is placed under the scalp during surgery; it holds the drugs as they flow through a small tube into the brain). The other way, shown in the bottom part of the figure, is to inject the drugs directly into the CSF in the lower part of the spinal column, after a small area on the lower back is numbed.
See Drugs Approved for Acute Lymphoblastic Leukemia for more information.
Learn more about how chemotherapy works, how it is given, common side effects, and more at Chemotherapy to Treat Cancer and Chemotherapy and You: Support for People with Cancer.
Radiation therapy
Radiation therapy uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer.
External radiation therapy may be used to treat ALL that has spread, or may spread, to the brain and spinal cord. When used this way, it is called central nervous system (CNS) sanctuary therapy or CNS prophylaxis. Total-body irradiation may be used to send radiation toward the whole body when preparing for a stem cell transplant. External radiation therapy may also be used as palliative therapy to relieve symptoms and improve quality of life.
Learn more about External Beam Radiation Therapy for Cancer and Radiation Therapy Side Effects.
Chemotherapy with stem cell transplant
Chemotherapy is given to kill cancer cells. Healthy cells, including blood-forming cells, are also destroyed by the cancer treatment. Stem cell transplant is a treatment to replace the blood-forming cells. Stem cells (immature blood cells) are removed from the blood or bone marrow of the patient or a donor and are frozen and stored. After the patient completes chemotherapy or total-body radiation therapy, the stored stem cells are thawed and given back to the patient through an infusion. These reinfused stem cells grow into (and restore) the body's blood cells.
Learn more about Stem Cell Transplants in Cancer Treatment.
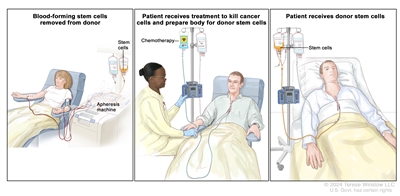
Donor stem cell transplant. (Step 1): Four to five days before donor stem cell collection, the donor receives a medicine to increase the number of stem cells circulating through their bloodstream (not shown). The blood-forming stem cells are then collected from the donor through a large vein in their arm. The blood flows through an apheresis machine that removes the stem cells. The rest of the blood is returned to the donor through a vein in their other arm. (Step 2): The patient receives chemotherapy to kill cancer cells and prepare their body for the donor stem cells. The patient may also receive radiation therapy (not shown). (Step 3): The patient receives an infusion of the donor stem cells.
Targeted therapy
Targeted therapy uses drugs or other substances to identify and attack specific cancer cells. Your doctor may suggest biomarker tests to help predict your response to certain targeted therapy drugs. Learn more about Biomarker Testing for Cancer.
Targeted therapies used to treat ALL include:
- dasatinib
- imatinib mesylate
- inotuzumab ozogamicin
- nilotinib
Learn more about Targeted Therapy to Treat Cancer.
Immunotherapy
Immunotherapy helps a person's immune system fight cancer. Your doctor may suggest biomarker tests to help predict your response to certain immunotherapy drugs. Learn more about Biomarker Testing for Cancer Treatment.
Immunotherapies used to treat ALL include:
- blinatumomab
- inotuzumab ozogamicin
- CAR T-cell therapy with brexucabtagene autoleucel or tisagenlecleucel
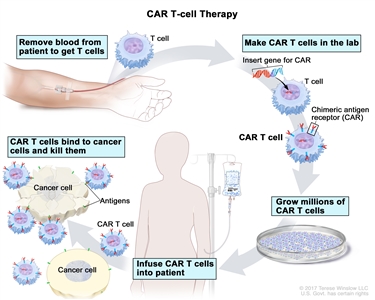
CAR T-cell therapy. A type of treatment in which a patient's T cells (a type of immune cell) are changed in the laboratory so they will bind to cancer cells and kill them. Blood from a vein in the patient's arm flows through a tube to an apheresis machine (not shown), which removes the white blood cells, including the T cells, and sends the rest of the blood back to the patient. Then, the gene for a special receptor called a chimeric antigen receptor (CAR) is inserted into the T cells in the laboratory. Millions of the CAR T cells are grown in the laboratory and then given to the patient by infusion. The CAR T cells are able to bind to an antigen on the cancer cells and kill them.
Learn more about Immunotherapy to Treat Cancer.
New types of treatment are being tested in clinical trials.
A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. For some patients, taking part in a clinical trial may be an option.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
To learn more about clinical trials, see Clinical Trials Information for Patients and Caregivers.
Treatment for ALL may cause side effects.
To learn more about side effects that begin during treatment for cancer, visit Side Effects.
Side effects from cancer treatment that begin after treatment and continue for months or years are called late effects. Late effects of treatment for ALL may include the risk of second cancers (new types of cancer). Regular follow-up exams are very important for long-term survivors.
Follow-up care may be needed.
As you go through treatment, you will have follow-up tests or check-ups. Some tests that were done to diagnose or stage the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back).
Treatment of Untreated Acute Lymphoblastic Leukemia
Treatment of ALL during the remission induction phase includes:
- combination chemotherapy
- targeted therapy with imatinib, in certain patients, some of whom will also have combination chemotherapy
- supportive care including antibiotics and red blood cell and platelet transfusions
- central nervous system (CNS) prophylaxis including chemotherapy (intrathecal and/or systemic) with or without radiation therapy to the brain
To learn more about these treatments, see the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Acute Lymphoblastic Leukemia in Remission
Treatment of ALL during the post-remission phase includes:
- chemotherapy
- targeted therapy with dasatinib, imatinib, or nilotinib
- chemotherapy with stem cell transplant
- central nervous system (CNS prophylaxis) including chemotherapy (intrathecal and/or systemic) with or without radiation therapy to the brain
To learn more about these treatments, see the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Recurrent Acute Lymphoblastic Leukemia
Treatment of recurrent ALL may include:
- combination chemotherapy followed by stem cell transplant
- immunotherapy (blinatumomab or inotuzumab ozogamicin) followed by stem cell transplant
- low-dose radiation therapy as palliative care to relieve symptoms and improve quality of life
- targeted therapy with dasatinib for certain patients
- CAR T-cell therapy (brexucabtagene autoleucel or tisagenlecleucel) for certain patients
Some of the treatments being studied in clinical trials for recurrent ALL include stem cell transplant using the patient's stem cells.
To learn more about these treatments, see the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
To Learn More About Acute Lymphoblastic Leukemia
For more information from the National Cancer Institute about ALL, visit the Leukemia Home Page.
For general cancer information and other resources from the National Cancer Institute, visit:
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of acute lymphoblastic leukemia. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Adult Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Acute Lymphoblastic Leukemia Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/leukemia/patient/adult-all-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389283]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2024-08-21
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.

