Thyroid Cancer Treatment (PDQ®): Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
General Information About Thyroid Cancer
Thyroid cancer is a disease in which malignant (cancer) cells form in the tissues of the thyroid gland.
The thyroid is a gland at the base of the throat near the trachea (windpipe). It is shaped like a butterfly, with a right lobe and a left lobe. The isthmus, a thin piece of tissue, connects the two lobes. A healthy thyroid is a little larger than a quarter. It usually cannot be felt through the skin.
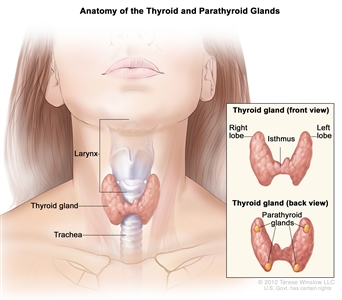
Anatomy of the thyroid and parathyroid glands. The thyroid gland lies at the base of the throat near the trachea. It is shaped like a butterfly, with the right lobe and left lobe connected by a thin piece of tissue called the isthmus. The parathyroid glands are four pea-sized organs found in the neck near the thyroid. The thyroid and parathyroid glands make hormones.
The thyroid uses iodine, a mineral found in some foods and in iodized salt, to help make several hormones. Thyroid hormones do the following:
- Control heart rate, body temperature, and how quickly food is changed into energy (metabolism).
- Control the amount of calcium in the blood.
Thyroid nodules are common but usually are not cancer.
Your doctor may find a lump (nodule) in your thyroid during a routine medical exam. A thyroid nodule is an abnormal growth of thyroid cells in the thyroid. Nodules may be solid or fluid -filled.
When a thyroid nodule is found, an ultrasound of the thyroid and a fine-needle aspiration biopsy are often done to check for signs of cancer. Blood tests to check thyroid hormone levels and for antithyroid antibodies in the blood may also be done to check for other types of thyroid disease.
Thyroid nodules usually don't cause symptoms or need treatment. Sometimes the thyroid nodules become large enough that it is hard to swallow or breathe and more tests and treatment are needed. Only a small number of thyroid nodules are diagnosed as cancer.
There are different types of thyroid cancer.
Thyroid cancer can be described as either:
- Differentiated thyroid cancer, which includes well-differentiated tumors, poorly differentiated tumors, and undifferentiated tumors; or
- Medullary thyroid cancer.
Well-differentiated tumors (papillary thyroid cancer and follicular thyroid cancer) can be treated and can usually be cured.
Poorly differentiated and undifferentiated tumors (anaplastic thyroid cancer) are less common. These tumors grow and spread quickly and have a poorer chance of recovery. Patients with anaplastic thyroid cancer should have molecular testing for a mutation in the BRAFgene.
Medullary thyroid cancer is a neuroendocrine tumor that develops in C cells of the thyroid. The C cells make a hormone (calcitonin) that helps maintain a healthy level of calcium in the blood.
For information about childhood thyroid cancer, see Childhood Thyroid Cancer Treatment.
Age, gender, and being exposed to radiation can affect the risk of thyroid cancer.
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn't mean that you will not get cancer. Talk with your doctor if you think you may be at risk.
Risk factors for thyroid cancer include the following:
- Being between 25 and 65 years old.
- Being female.
- Being exposed to radiation to the head and neck as an infant or child or being exposed to radioactive fallout. The cancer may occur as soon as 5 years after exposure.
- Having a history of goiter (enlarged thyroid).
- Having a family history of thyroid disease or thyroid cancer.
- Having certain genetic conditions such as familial medullary thyroid cancer (FMTC), multiple endocrine neoplasia type 2A syndrome (MEN2A), or multiple endocrine neoplasia type 2B syndrome (MEN2B).
- Being Asian.
Medullary thyroid cancer is sometimes caused by a change in a gene that is passed from parent to child.
The genes in cells carry hereditary information from parent to child. A certain change in the RET gene that is passed from parent to child (inherited) may cause medullary thyroid cancer.
There is a genetic test that is used to check for the changed gene. The patient is tested first to see if he or she has the changed gene. If the patient has it, other family members may also be tested to find out if they are at increased risk for medullary thyroid cancer. Family members, including young children, who have the changed gene may have a thyroidectomy (surgery to remove the thyroid). This can decrease the chance of developing medullary thyroid cancer.
Signs of thyroid cancer include a swelling or lump in the neck.
Thyroid cancer may not cause early signs or symptoms. It is sometimes found during a routine physical exam. Signs or symptoms may occur as the tumor gets bigger. Other conditions may cause the same signs or symptoms. Check with your doctor if you have any of the following:
- A lump (nodule) in the neck.
- Trouble breathing.
- Trouble swallowing.
- Pain when swallowing.
- Hoarseness.
Tests that examine the thyroid, neck, and blood are used to diagnose thyroid cancer.
The following tests and procedures may be used:
- Physical exam and health history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps (nodules) or swelling in the neck, voice box, and lymph nodes, and anything else that seems unusual. A history of the patient's health habits and past illnesses and treatments will also be taken.
- Laryngoscopy: A procedure in which the doctor checks the larynx (voice box) with a mirror or a laryngoscope. A laryngoscope is a thin, tube-like instrument with a light and a lens for viewing. A thyroid tumor may press on vocal cords. The laryngoscopy is done to see if the vocal cords are moving normally.
- Blood hormone studies: A procedure in which a blood sample is checked to measure the amounts of certain hormones released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. The blood may be checked for abnormal levels of thyroid-stimulating hormone (TSH). TSH is made by the pituitary gland in the brain. It stimulates the release of thyroid hormone and controls how fast follicular thyroid cells grow. The blood may also be checked for high levels of the hormone calcitonin and antithyroid antibodies.
- Blood chemistry studies: A procedure in which a blood sample is checked to measure the amounts of certain substances, such as calcium, released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease.
- Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs in the neck and make echoes. The echoes form a picture of body tissues called a sonogram. The picture can be printed to be looked at later. This procedure can show the size of a thyroid nodule and whether it is solid or a fluid-filled cyst. Ultrasound may be used to guide a fine-needle aspiration biopsy.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, such as the neck, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
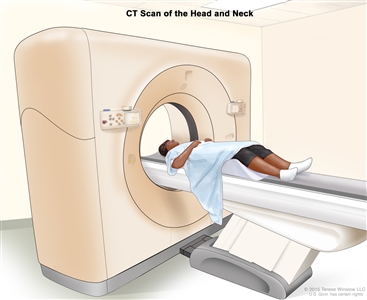
Computed tomography (CT) scan of the head and neck. The patient lies on a table that slides through the CT scanner, which takes x-ray pictures of the inside of the head and neck. - Fine-needle aspiration biopsy of the thyroid: The removal of thyroid tissue using a thin needle. The needle is inserted through the skin into the thyroid. Several tissue samples are removed from different parts of the thyroid. A pathologist views the tissue samples under a microscope to look for cancer cells. Because the type of thyroid cancer can be hard to diagnose, patients should ask to have biopsy samples checked by a pathologist who has experience diagnosing thyroid cancer.
- Surgical biopsy: The removal of the thyroid nodule or one lobe of the thyroid during surgery so the cells and tissues can be viewed under a microscope by a pathologist to check for signs of cancer. Because the type of thyroid cancer can be hard to diagnose, patients should ask to have biopsy samples checked by a pathologist who has experience diagnosing thyroid cancer.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis and treatment options depend on the following:
- The age of the patient at the time of diagnosis.
- The type of thyroid cancer.
- The stage of the cancer.
- Whether the cancer was completely removed by surgery.
- Whether the patient has multiple endocrine neoplasia type 2B (MEN 2B).
- The patient's general health.
- Whether the cancer has just been diagnosed or has recurred (come back).
Stages of Thyroid Cancer
After thyroid cancer has been diagnosed, tests are done to find out if cancer cells have spread within the thyroid or to other parts of the body.
The process used to find out if cancer has spread within the thyroid or to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the patient's age and the stage of the cancer to plan treatment.
The following tests and procedures may be used in the staging process:
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, such as the chest, abdomen, and brain, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. The picture can be printed to be looked at later.
- Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- Bone scan: A procedure to check if there are rapidly dividing cells, such as cancer cells, in the bone. A very small amount of radioactive material is injected into a vein and travels through the bloodstream. The radioactive material collects in the bones with cancer and is detected by a scanner.
- Sentinel lymph node biopsy: The removal of the sentinel lymph node during surgery. The sentinel lymph node is the first lymph node in a group of lymph nodes to receive lymphatic drainage from the primary tumor. It is the first lymph node the cancer is likely to spread to from the primary tumor. A radioactive substance and/or blue dye is injected near the tumor. The substance or dye flows through the lymph ducts to the lymph nodes. The first lymph node to receive the substance or dye is removed. A pathologist views the tissue under a microscope to look for cancer cells. If cancer cells are not found, it may not be necessary to remove more lymph nodes.
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
Cancer may spread from where it began to other parts of the body.
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began (the primary tumor) and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor (metastatic tumor) in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumor (metastatic tumor) in another part of the body.
The metastatic tumor is the same type of cancer as the primary tumor. For example, if thyroid cancer spreads to the lung, the cancer cells in the lung are actually thyroid cancer cells. The disease is metastatic thyroid cancer, not lung cancer.
Stages are used to describe thyroid cancer based on the type of thyroid cancer and the age of the patient:
Papillary and follicular thyroid cancer in patients younger than 55 years
- Stage I: In stage I papillary and follicular thyroid cancer, the tumor is any size and may have spread to nearby tissues and lymph nodes. Cancer has not spread to other parts of the body.
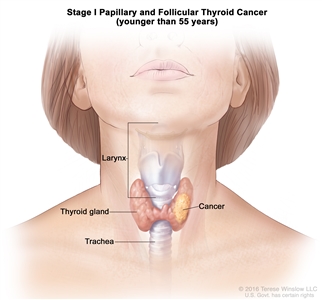
Stage I papillary and follicular thyroid cancer in patients younger than 55 years. The tumor is any size and cancer may have spread to nearby tissues and lymph nodes. Cancer has not spread to other parts of the body. - Stage II: In stage II papillary and follicular thyroid cancer, the tumor is any size and cancer may have spread to nearby tissues and lymph nodes. Cancer has spread from the thyroid to other parts of the body, such as the lungs or bones.
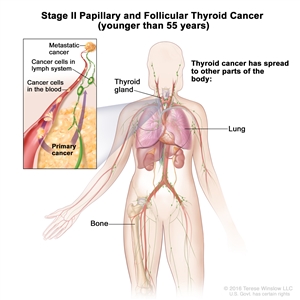
Stage II papillary and follicular thyroid cancer in patients younger than 55 years. The tumor is any size and cancer may have spread to nearby tissues and lymph nodes. Cancer has spread from the thyroid to other parts of the body, such as the lungs or bones.
Papillary and follicular thyroid cancer in patients 55 years and older
- Stage I: In stage I papillary and follicular thyroid cancer, cancer is found in the thyroid only and the tumor is 4 centimeters or smaller.
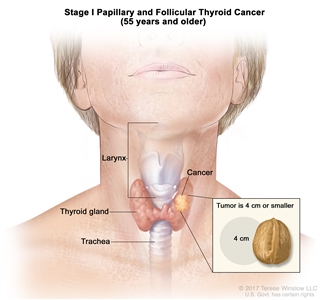
Stage I papillary and follicular thyroid cancer in patients 55 years and older. Cancer is found in the thyroid only and the tumor is 4 centimeters or smaller. - Stage II: In stage II papillary and follicular thyroid cancer, one of the following is found:
- cancer is found in the thyroid and the tumor is 4 centimeters or smaller; cancer has spread to nearby lymph nodes; or
- cancer is found in the thyroid, the tumor is larger than 4 centimeters, and cancer may have spread to nearby lymph nodes; or
- the tumor is any size and cancer has spread from the thyroid to nearby muscles in the neck and may have spread to nearby lymph nodes.
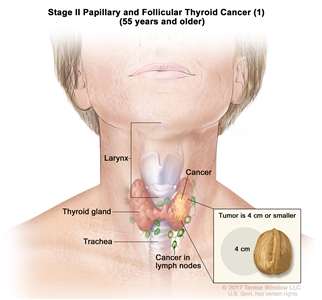
Stage II papillary and follicular thyroid cancer (1) in patients 55 years and older. Cancer is found in the thyroid and the tumor is 4 centimeters or smaller. Cancer has spread to nearby lymph nodes. - Stage III: In stage III papillary and follicular thyroid cancer, the tumor is any size and cancer has spread from the thyroid to soft tissue under the skin, the esophagus, the trachea, the larynx, or the recurrent laryngeal nerve (a nerve that goes to the larynx). Cancer may have spread to lymph nodes.
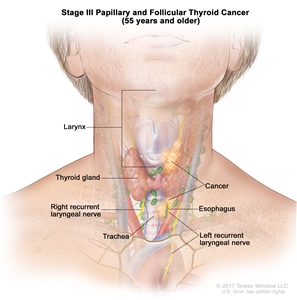
Stage III papillary and follicular thyroid cancer in patients 55 years and older. The tumor is any size and cancer has spread from the thyroid to soft tissue under the skin, the esophagus, the trachea, the larynx, or the recurrent laryngeal nerve (a nerve that goes to the larynx). Cancer may have spread to lymph nodes. - Stage IV: Stage IV papillary and follicular thyroid cancer is divided into stages IVA and IVB.
- In stage IVA, the tumor is any size and cancer has spread to tissue in front of the spine or has surrounded the carotid artery or the blood vessels in the area between the lungs. Cancer may have spread to lymph nodes.
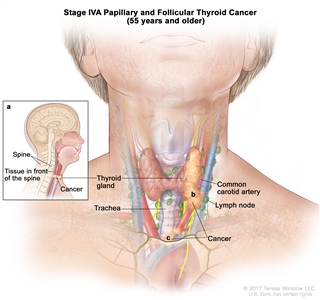
Stage IVA papillary and follicular thyroid cancer in patients 55 years and older. The tumor is any size and cancer has (a) spread to tissue in front of the spine; or (b) surrounded the carotid artery; or (c) surrounded the blood vessels in the area between the lungs. Cancer may have spread to lymph nodes. - In stage IVB, the tumor is any size and cancer has spread to other parts of the body, such as the lungs or bones. Cancer may have spread to lymph nodes.
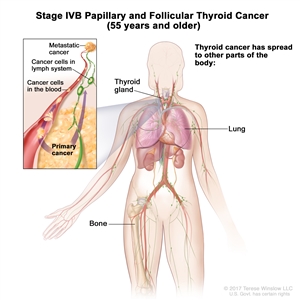
Stage IVB papillary and follicular thyroid cancer in patients 55 years and older. The tumor is any size and cancer has spread to other parts of the body, such as the lungs or bones. Cancer may have spread to lymph nodes.
- In stage IVA, the tumor is any size and cancer has spread to tissue in front of the spine or has surrounded the carotid artery or the blood vessels in the area between the lungs. Cancer may have spread to lymph nodes.
Anaplastic thyroid cancer in patients of all ages
Anaplastic thyroid cancer grows quickly and usually has spread within the neck when it is found. Anaplastic thyroid cancer is considered stage IV thyroid cancer. Stage IV anaplastic thyroid cancer is divided into stages IVA, IVB, and IVC.
- In stage IVA, cancer is found in the thyroid only and the tumor may be any size.
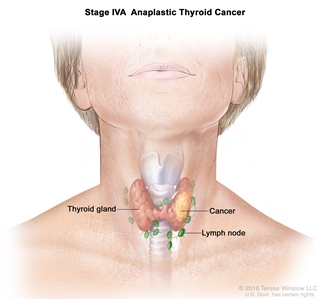
Stage IVA anaplastic thyroid cancer. Cancer is found in the thyroid only and the tumor may be any size. - In stage IVB, one of the following is found:
- cancer is found in the thyroid and the tumor may be any size; cancer has spread to nearby lymph nodes; or
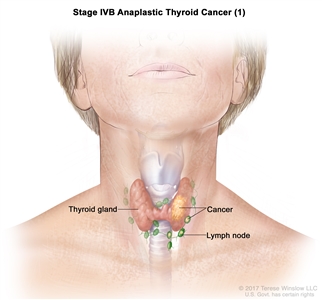
Stage IVB anaplastic thyroid cancer (1). Cancer is found in the thyroid and the tumor may be any size. Cancer has spread to nearby lymph nodes. - the tumor is any size and cancer has spread from the thyroid to nearby muscles in the neck and may have spread to nearby lymph nodes; or
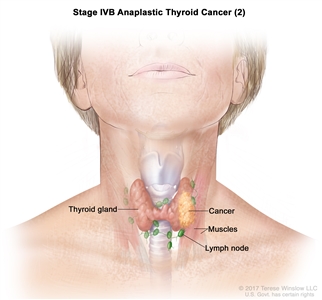
Stage IVB anaplastic thyroid cancer (2). The tumor is any size and cancer has spread from the thyroid to nearby muscles in the neck. Cancer may have spread to nearby lymph nodes. - the tumor is any size and cancer has spread from the thyroid to soft tissue under the skin, the esophagus, the trachea, the larynx, the recurrent laryngeal nerve (a nerve that goes to the larynx), or tissue in front of the spine, or has surrounded the carotid artery or the blood vessels in the area between the lungs; cancer may have spread to lymph nodes.
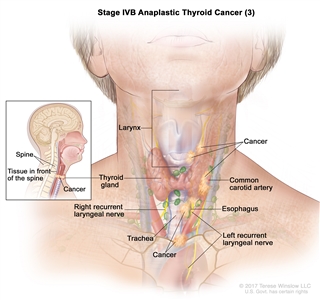
Stage IVB anaplastic thyroid cancer (3). The tumor is any size and cancer has spread from the thyroid to soft tissue under the skin, the esophagus, the trachea, the larynx, the recurrent laryngeal nerve (a nerve that goes to the larynx), or tissue in front of the spine; or cancer has surrounded the carotid artery or the blood vessels in the area between the lungs. Cancer may have spread to lymph nodes.
- cancer is found in the thyroid and the tumor may be any size; cancer has spread to nearby lymph nodes; or
- In stage IVC, the tumor is any size and cancer has spread to other parts of the body, such as the lungs or bones. Cancer may have spread to lymph nodes.
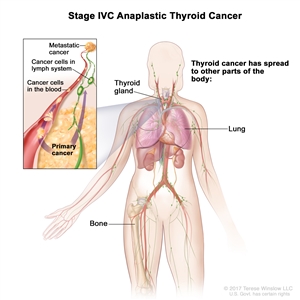
Stage IVC anaplastic thyroid cancer. The tumor is any size and cancer has spread to other parts of the body, such as the lungs or bones. Cancer may have spread to lymph nodes.
Medullary thyroid cancer in patients of all ages
- Stage I: In stage I medullary thyroid cancer, cancer is found in the thyroid only and the tumor is 2 centimeters or smaller.
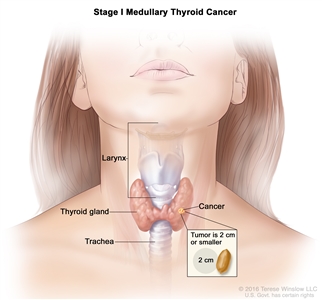
Stage I medullary thyroid cancer. Cancer is found in the thyroid only and the tumor is 2 centimeters or smaller. - Stage II: In stage II medullary thyroid cancer, one of the following is found:
- cancer is in the thyroid only and the tumor is larger than 2 centimeters; or
- the tumor is any size and cancer has spread from the thyroid to nearby muscles in the neck.
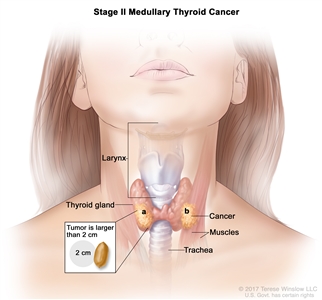
Stage II medullary thyroid cancer. The cancer (a) is found in the thyroid only and the tumor is larger than 2 centimeters; or (b) has spread from the thyroid to nearby muscles in the neck and the tumor is any size. - Stage III: In stage III medullary thyroid cancer, the tumor is any size and cancer may have spread from the thyroid to nearby muscles in the neck. Cancer has spread to lymph nodes on one or both sides of the trachea or larynx.
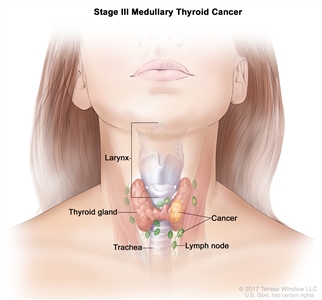
Stage III medullary thyroid cancer. The tumor is any size and cancer may have spread from the thyroid to nearby muscles in the neck. Cancer has spread to lymph nodes on one or both sides of the trachea or larynx. - Stage IV: Stage IV medullary thyroid cancer is divided into stages IVA, IVB, and IVC.
- In stage IVA, either of the following is found:
- the tumor is any size and cancer has spread from the thyroid to soft tissue under the skin, the esophagus, the trachea, the larynx, or the recurrent laryngeal nerve (a nerve that goes to the larynx); cancer may have spread to lymph nodes on one or both sides of the neck; or
- the tumor is any size and cancer may have spread from the thyroid to nearby muscles in the neck; cancer has spread to lymph nodes on one or both sides of the neck.
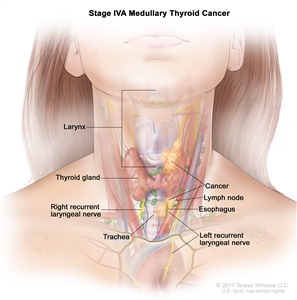
Stage IVA medullary thyroid cancer. The tumor is any size and cancer has spread from the thyroid to soft tissue under the skin, the esophagus, the trachea, the larynx, or the recurrent laryngeal nerve (a nerve that goes to the larynx), and cancer may have spread to lymph nodes on one or both sides of the neck; or cancer may have spread from the thyroid to nearby muscles in the neck, and cancer has spread to lymph nodes on one or both sides of the neck.
- In stage IVA, either of the following is found:
- In stage IVB, the tumor is any size and cancer has spread to tissue in front of the spine or to the spine or has surrounded the carotid artery or the blood vessels in the area between the lungs. Cancer may have spread to lymph nodes.
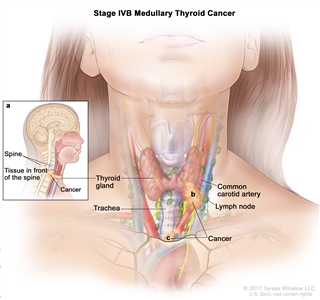
Stage IVB medullary thyroid cancer. The tumor is any size and cancer has (a) spread to tissue in front of the spine or to the spine; or (b) surrounded the carotid artery; or (c) surrounded the blood vessels in the area between the lungs. Cancer may have spread to lymph nodes. - In stage IVC, the tumor is any size and cancer has spread to other parts of the body, such as the lungs or liver. Cancer may have spread to lymph nodes.
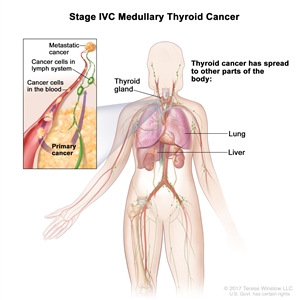
Stage IVC medullary thyroid cancer. The tumor is any size and cancer has spread to other parts of the body, such as the lung or liver. Cancer may have spread to lymph nodes.
Thyroid cancer can recur (come back) after it has been treated.
The cancer may come back in the thyroid or in other parts of the body.
Treatment Option Overview
There are different types of treatment for patients with thyroid cancer.
Different types of treatment are available for patients with thyroid cancer. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
The following types of treatment are used:
Surgery
Surgery is the most common treatment for thyroid cancer. One of the following procedures may be used:
- Lobectomy: Removal of the lobe in which thyroid cancer is found. Lymph nodes near the cancer may also be removed and checked under a microscope for signs of cancer.
- Near-total thyroidectomy: Removal of all but a very small part of the thyroid. Lymph nodes near the cancer may also be removed and checked under a microscope for signs of cancer.
- Total thyroidectomy: Removal of the whole thyroid. Lymph nodes near the cancer may also be removed and checked under a microscope for signs of cancer.
- Tracheostomy: Surgery to create an opening (stoma) into the windpipe to help you breathe. The opening itself may also be called a tracheostomy.
Radiation therapy, including radioactive iodine therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer. Sometimes the radiation is aimed directly at the tumor during surgery. This is called intraoperative radiation therapy.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
Radiation therapy may be given after surgery to kill any thyroid cancer cells that were not removed. Follicular and papillary thyroid cancers are sometimes treated with radioactive iodine (RAI) therapy. RAI is taken by mouth and collects in any remaining thyroid tissue, including thyroid cancer cells that have spread to other places in the body. Since only thyroid tissue takes up iodine, the RAI destroys thyroid tissue and thyroid cancer cells without harming other tissue. Before a full treatment dose of RAI is given, a small test-dose is given to see if the tumor takes up the iodine.
The way the radiation therapy is given depends on the type and stage of the cancer being treated. External radiation therapy and radioactive iodine (RAI) therapy are used to treat thyroid cancer.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy).
The way the chemotherapy is given depends on the type and stage of the cancer being treated.
See Drugs Approved for Thyroid Cancer for more information.
Thyroid hormone therapy
Hormone therapy is a cancer treatment that removes hormones or blocks their action and stops cancer cells from growing. Hormones are substances made by glands in the body and circulated in the bloodstream. In the treatment of thyroid cancer, drugs may be given to prevent the body from making thyroid-stimulating hormone (TSH), a hormone that can increase the chance that thyroid cancer will grow or recur.
Also, because thyroid cancer treatment kills thyroid cells, the thyroid is not able to make enough thyroid hormone. Patients are given thyroid hormone replacement pills.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. There are different types of targeted therapy:
- Tyrosine kinase inhibitor. Tyrosine kinase inhibitor therapy blocks signals needed for tumors to grow. Sorafenib, lenvatinib, vandetanib, cabozantinib, selpercatinib, larotrectinib, entrectinib, and pralsetinib are used to treat certain types of thyroid cancer. New types of tyrosine kinase inhibitors are being studied to treat advanced thyroid cancer.
- Protein kinase inhibitor. Protein kinase inhibitor therapy blocks proteins needed for cell growth and may kill cancer cells. Dabrafenib and trametinib are used to treat anaplastic thyroid cancer in patients with a certain mutation in the BRAFgene.
See Drugs Approved for Thyroid Cancer for more information.
Watchful waiting
Watchful waiting is closely monitoring a patient's condition without giving any treatment until signs or symptoms appear or change.
New types of treatment are being tested in clinical trials.
Immunotherapy
Immunotherapy is a treatment that uses the patient's immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body's natural defenses against cancer. This cancer treatment is a type of biologic therapy. Immunotherapy is being studied as a treatment for thyroid cancer.
Information about clinical trials is available from the NCI website.
Treatment for thyroid cancer may cause side effects.
For information about side effects caused by treatment for cancer, visit our Side Effects page.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials supported by NCI can be found on NCI's clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Follow-up tests may be needed.
As you go through treatment, you will have follow-up tests or check-ups. Some tests that were done to diagnose or stage the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back).
Treatment of Stages I, II, and III Papillary and Follicular Thyroid Cancer (Localized / Regional)
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of stage I (younger than 55 years; 55 years and older), stage II (younger than 55 years; 55 years and older), and stage III papillary and follicular thyroid cancer may include the following:
- Surgery (thyroidectomy or lobectomy).
- Radioactive iodine therapy.
- Hormone therapy to prevent the body from making thyroid-stimulating hormone (TSH).
- External radiation therapy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Stage IV Papillary and Follicular Thyroid Cancer (Metastatic)
For information about the treatments listed below, see the Treatment Option Overview section.
When cancer has spread to other places in the body, such as the lungs and bone, treatment usually does not cure the cancer, but can relieve symptoms and improve the quality of life. Treatment of stage IV papillary and follicular thyroid cancer may include the following:
For tumors that take up iodine
- Total thyroidectomy.
- Radioactive iodine therapy.
- Hormone therapy to prevent the body from making thyroid-stimulating hormone (TSH).
For tumors that do not take up iodine
- Total thyroidectomy.
- Hormone therapy to prevent the body from making thyroid-stimulating hormone (TSH).
- Targeted therapy with a tyrosine kinase inhibitor (sorafenib or lenvatinib).
- Surgery to remove cancer from areas where it has spread.
- External-beam radiation therapy.
- A clinical trial of chemotherapy.
- A clinical trial of a targeted therapy.
- A clinical trial of immunotherapy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Recurrent Papillary and Follicular Thyroid Cancer
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of recurrent papillary and follicular thyroid cancer may include the following:
- Surgery to remove the tumor with or without radioactive iodine therapy.
- Radioactive iodine therapy when the cancer can be found only by a thyroid scan and cannot be felt during a physical exam.
- Targeted therapy with a tyrosine kinase inhibitor (sorafenib, lenvatinib, cabozantinib, selpercatinib, pralsetinib, larotrectinib, or entrectinib).
- External radiation therapy or intraoperative radiation therapy as palliative therapy to relieve symptoms and improve the quality of life.
- Chemotherapy.
- A clinical trial of a targeted therapy.
- A clinical trial of immunotherapy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Medullary Thyroid Cancer
For information about the treatments listed below, see the Treatment Option Overview section.
Localized medullary thyroid cancer is in the thyroid only and may have spread to nearby muscles in the neck. Locally advanced and metastatic thyroid cancer has spread to other parts of the neck or to other parts of the body.
Treatment of localized medullary thyroid cancer may include the following:
- Total thyroidectomy if the cancer has not spread to other parts of the body. Lymph nodes near the cancer are also removed.
- External radiation therapy for patients whose cancer has recurred in the thyroid.
Treatment of locally advanced/metastatic medullary thyroid cancer may include the following:
- Targeted therapy with a tyrosine kinase inhibitor (vandetanib, cabozantinib, or selpercatinib) for cancer that has spread to other parts of the body.
- Chemotherapy as palliative therapy to relieve symptoms and improve the quality of life for patients whose cancer has spread to other parts of the body.
Radioactive iodine therapy is not used to treat medullary thyroid cancer.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Anaplastic Thyroid Cancer
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of anaplastic thyroid cancer may include the following:
- Total thyroidectomy as palliative therapy to relieve symptoms and improve the quality of life for patients whose cancer is in or near the thyroid.
- Tracheostomy as palliative therapy to relieve symptoms and improve the quality of life.
- External radiation therapy.
- Chemotherapy.
- Targeted therapy with protein kinase inhibitors (dabrafenib and trametinib) for patients with a certain mutation in the BRAFgene.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
To Learn More About Thyroid Cancer
For more information from the National Cancer Institute about thyroid cancer, see the following:
- Thyroid Cancer Home Page
- Drugs Approved for Thyroid Cancer
- Targeted Cancer Therapies
- Immunotherapy to Treat Cancer
- Genetic Testing for Inherited Cancer Susceptibility Syndromes
For general cancer information and other resources from the National Cancer Institute, visit:
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of adult thyroid cancer. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Adult Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Thyroid Cancer Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/thyroid/patient/thyroid-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389296]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2023-07-21
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.

