Breast Cancer Treatment During Pregnancy (PDQ®): Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
General Information About Breast Cancer Treatment During Pregnancy
Breast cancer is a disease in which malignant (cancer) cells form in the tissues of the breast.
The breast is made up of lobes and ducts. Each breast has 15 to 20 sections called lobes. Each lobe has many smaller sections called lobules. Lobules end in dozens of tiny bulbs that can make milk. The lobes, lobules, and bulbs are linked by thin tubes called ducts. 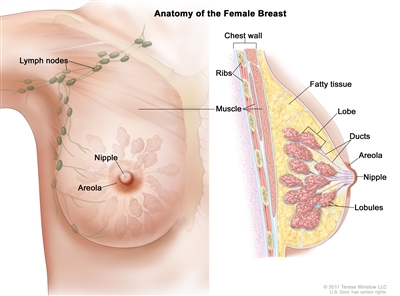
Anatomy of the female breast. The nipple and areola are shown on the outside of the breast. The lymph nodes, lobes, lobules, ducts, and other parts of the inside of the breast are also shown.
Each breast also has blood vessels and lymph vessels. The lymph vessels carry an almost colorless, watery fluid called lymph. Lymph vessels carry lymph between lymph nodes. Lymph nodes are small, bean-shaped structures found throughout the body. They filter lymph and store white blood cells that help fight infection and disease. Groups of lymph nodes are found near the breast in the axilla (under the arm), above the collarbone, and in the chest.
Sometimes breast cancer occurs in women who are pregnant or have just given birth.
Breast cancer occurs about once in every 3,000 pregnancies. It occurs most often in women aged 32 to 38 years. Because many women are choosing to delay having children, it is likely that the number of new cases of breast cancer during pregnancy will increase.
Signs of breast cancer include a lump or change in the breast.
These and other signs may be caused by breast cancer or by other conditions. Check with your doctor if you have any of the following:
- A lump or thickening in or near the breast or in the underarm area.
- A change in the size or shape of the breast.
- A dimple or puckering in the skin of the breast.
- A nipple turned inward into the breast.
- Fluid, other than breast milk, from the nipple, especially if it's bloody.
- Scaly, red, or swollen skin on the breast, nipple, or areola (the dark area of skin around the nipple).
- Dimples in the breast that look like the skin of an orange, called peau d'orange.
It may be difficult to detect (find) breast cancer early in pregnant or nursing women.
The breasts usually get larger, tender, or lumpy in women who are pregnant, nursing, or have just given birth. This occurs because of normal hormone changes that take place during pregnancy. These changes can make small lumps difficult to detect. The breasts may also become denser. It is more difficult to detect breast cancer in women with dense breasts using mammography. Because these breast changes can delay diagnosis, breast cancer is often found at a later stage in these women.
Breast exams should be part of prenatal and postnatal care.
To detect breast cancer, pregnant and nursing women should examine their breasts themselves. Women should also receive clinical breast exams during their regular prenatal and postnatal check-ups. Talk to your doctor if you notice any changes in your breasts that you do not expect or that worry you.
Tests that examine the breasts are used to diagnose breast cancer.
The following tests and procedures may be used:
- Physical exam and health history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient's health habits and past illnesses and treatments will also be taken.
- Clinical breast exam (CBE): An exam of the breast by a doctor or other health professional. The doctor will carefully feel the breasts and under the arms for lumps or anything else that seems unusual.
- Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram. The picture can be printed to look at later.
- Mammogram: An x-ray of the breast. A mammogram can be done with little risk to the fetus. Mammograms in pregnant women may appear negative even though cancer is present.
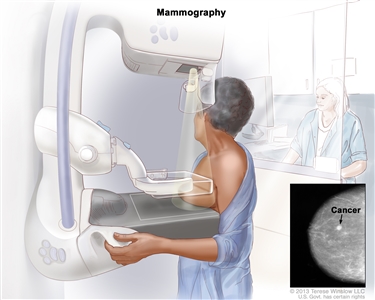
Mammography. The breast is pressed between two plates. X-rays are used to take pictures of breast tissue. - Biopsy: The removal of cells or tissues so they can be viewed under a microscope by a pathologist to check for signs of cancer. If a lump in the breast is found, a biopsy may be done.
There are three types of breast biopsies:
- Excisional biopsy: The removal of an entire lump of tissue.
- Core biopsy: The removal of tissue using a wide needle.
- Fine-needle aspiration (FNA) biopsy: The removal of tissue or fluid, using a thin needle.
If cancer is found, tests are done to study the cancer cells.
Decisions about the best treatment are based on the results of these tests and the trimester of the pregnancy. The tests give information about:
- How quickly the cancer may grow.
- How likely it is that the cancer will spread to other parts of the body.
- How well certain treatments might work.
- How likely the cancer is to recur (come back).
Tests may include the following:
- Estrogen and progesterone receptor test: A test to measure the amount of estrogen and progesterone (hormones) receptors in cancer tissue. If there are more estrogen or progesterone receptors than normal, the cancer is called estrogen receptor positive or progesterone receptor positive. This type of breast cancer may grow more quickly. The test results show whether treatment to block estrogen and progesterone given after the baby is born may stop the cancer from growing.
- Human epidermal growth factor type 2 receptor (HER2/neu) test: A laboratory test to measure how many HER2/neugenes there are and how much HER2/neu protein is made in a sample of tissue. If there are more HER2/neu genes or higher levels of HER2/neu protein than normal, the cancer is called HER2/neu positive. This type of breast cancer may grow more quickly and is more likely to spread to other parts of the body. The cancer may be treated with drugs that target the HER2/neu protein, such as trastuzumab and pertuzumab, after the baby is born.
- Multigene tests: Tests in which samples of tissue are studied to look at the activity of many genes at the same time. These tests may help predict whether cancer will spread to other parts of the body or recur (come back).
- Oncotype DX: This test helps predict whether stage I or stage II breast cancer that is estrogen receptor positive and node-negative will spread to other parts of the body. If the risk of the cancer spreading is high, chemotherapy may be given to lower the risk.
- MammaPrint: A laboratory test in which the activity of 70 different genes is looked at in the breast cancer tissue of women who have early-stage invasive breast cancer that has not spread to lymph nodes or has spread to 3 or fewer lymph nodes. The activity level of these genes helps predict whether breast cancer will spread to other parts of the body or come back. If the test shows that the risk that the cancer will spread or come back is high, chemotherapy may be given to lower the risk.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis and treatment options depend on the following:
- The stage of the cancer (the size of the tumor and whether it is in the breast only or has spread to other parts of the body).
- The type of breast cancer.
- The trimester of the pregnancy.
- Whether there are signs or symptoms.
- The patient's general health.
Stages of Breast Cancer
After breast cancer has been diagnosed, tests are done to find out if cancer cells have spread within the breast or to other parts of the body.
The process used to find out if the cancer has spread within the breast or to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the stage in order to plan treatment.
Some procedures may expose the fetus to harmful radiation or dyes. These procedures are done only if absolutely necessary. Certain actions, such as using a lead-lined shield to cover the abdomen, are used to help protect the fetus from radiation as much as possible.
The following tests and procedures may be used to stage breast cancer during pregnancy:
- Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- Bone scan: A procedure to check if there are rapidly dividing cells, such as cancer cells, in the bone. A very small amount of radioactive material is injected into a vein and travels through the bloodstream. The radioactive material collects in bones with cancer and is detected by a scanner.
- Ultrasound exam: A procedure in which high-energy sound waves (ultrasound) are bounced off internal tissues or organs, such as the liver, and make echoes. The echoes form a picture of body tissues called a sonogram. The picture can be printed to be looked at later.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body, such as the brain. This procedure is also called nuclear magnetic resonance imaging (NMRI).
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
Cancer may spread from where it began to other parts of the body.
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began (the primary tumor) and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor (metastatic tumor) in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumor (metastatic tumor) in another part of the body.
The metastatic tumor is the same type of cancer as the primary tumor. For example, if breast cancer spreads to the bone, the cancer cells in the bone are actually breast cancer cells. The disease is metastatic breast cancer, not bone cancer.
In breast cancer, stage is based on the size and location of the primary tumor, the spread of cancer to nearby lymph nodes or other parts of the body, tumor grade, and whether certain biomarkers are present.
To plan the best treatment and understand your prognosis, it is important to know the breast cancer stage.
There are 3 types of breast cancer stage groups:
- Clinical Prognostic Stage is used first to assign a stage for all patients based on health history, physical exam, imaging tests (if done), and biopsies. The Clinical Prognostic Stage is described by the TNM system, tumor grade, and biomarker status (ER, PR, HER2). In clinical staging, mammography or ultrasound is used to check the lymph nodes for signs of cancer.
- Pathological Prognostic Stage is then used for patients who have surgery as their first treatment. The Pathological Prognostic Stage is based on all clinical information, biomarker status, and laboratory test results from breast tissue and lymph nodes removed during surgery.
- Anatomic Stage is based on the size and the spread of cancer as described by the TNM system. The Anatomic Stage is used in parts of the world where biomarker testing is not available. It is not used in the United States.
The TNM system is used to describe the size of the primary tumor and the spread of cancer to nearby lymph nodes or other parts of the body.
For breast cancer, the TNM system describes the tumor as follows:
Tumor (T). The size and location of the tumor.
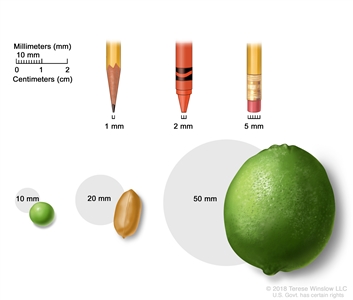
Tumor sizes are often measured in millimeters (mm) or centimeters. Common items that can be used to show tumor size in mm include: a sharp pencil point (1 mm), a new crayon point (2 mm), a pencil-top eraser (5 mm), a pea (10 mm), a peanut (20 mm), and a lime (50 mm).
- TX: Primary tumor cannot be assessed.
- T0: No sign of a primary tumor in the breast.
- Tis: Carcinoma in situ. There are 2 types of breast carcinoma in situ:
- Tis (DCIS): DCIS is a condition in which abnormal cells are found in the lining of a breast duct. The abnormal cells have not spread outside the duct to other tissues in the breast. In some cases, DCIS may become invasive breast cancer that is able to spread to other tissues. At this time, there is no way to know which lesions can become invasive.
- Tis (Paget disease): Paget disease of the nipple is a condition in which abnormal cells are found in the skin cells of the nipple and may spread to the areola. It is not staged according to the TNM system. If Paget disease AND an invasive breast cancer are present, the TNM system is used to stage the invasive breast cancer.
- T1: The tumor is 20 millimeters or smaller. There are 4 subtypes of a T1 tumor depending on the size of the tumor:
- T1mi: the tumor is 1 millimeter or smaller.
- T1a: the tumor is larger than 1 millimeter but not larger than 5 millimeters.
- T1b: the tumor is larger than 5 millimeters but not larger than 10 millimeters.
- T1c: the tumor is larger than 10 millimeters but not larger than 20 millimeters.
- T2: The tumor is larger than 20 millimeters but not larger than 50 millimeters.
- T3: The tumor is larger than 50 millimeters.
- T4: The tumor is described as one of the following:
- T4a: the tumor has grown into the chest wall.
- T4b: the tumor has grown into the skin—an ulcer has formed on the surface of the skin on the breast, small tumor nodules have formed in the same breast as the primary tumor, and/or there is swelling of the skin on the breast.
- T4c: the tumor has grown into the chest wall and the skin.
- T4d: inflammatory breast cancer —one-third or more of the skin on the breast is red and swollen (called peau d'orange).
Lymph Node (N). The size and location of lymph nodes where cancer has spread.
When the lymph nodes are removed by surgery and studied under a microscope by a pathologist, pathologic staging is used to describe the lymph nodes. The pathologic staging of lymph nodes is described below.
- NX: The lymph nodes cannot be assessed.
- N0: No sign of cancer in the lymph nodes, or tiny clusters of cancer cells not larger than 0.2 millimeters in the lymph nodes.
- N1: Cancer is described as one of the following:
- N1mi: cancer has spread to the axillary (armpit area) lymph nodes and is larger than 0.2 millimeters but not larger than 2 millimeters.
- N1a: cancer has spread to 1 to 3 axillary lymph nodes and the cancer in at least one of the lymph nodes is larger than 2 millimeters.
- N1b: cancer has spread to lymph nodes near the breastbone on the same side of the body as the primary tumor, and the cancer is larger than 0.2 millimeters and is found by sentinel lymph node biopsy. Cancer is not found in the axillary lymph nodes.
- N1c: cancer has spread to 1 to 3 axillary lymph nodes and the cancer in at least one of the lymph nodes is larger than 2 millimeters. Cancer is also found by sentinel lymph node biopsy in the lymph nodes near the breastbone on the same side of the body as the primary tumor.
- N2: Cancer is described as one of the following:
- N2a: cancer has spread to 4 to 9 axillary lymph nodes and the cancer in at least one of the lymph nodes is larger than 2 millimeters.
- N2b: cancer has spread to lymph nodes near the breastbone and the cancer is found by imaging tests. Cancer is not found in the axillary lymph nodes by sentinel lymph node biopsy or lymph node dissection.
- N3: Cancer is described as one of the following:
- N3a: cancer has spread to 10 or more axillary lymph nodes and the cancer in at least one of the lymph nodes is larger than 2 millimeters, or cancer has spread to lymph nodes below the collarbone.
- N3b: cancer has spread to 1 to 9 axillary lymph nodes and the cancer in at least one of the lymph nodes is larger than 2 millimeters. Cancer has also spread to lymph nodes near the breastbone and the cancer is found by imaging tests;
or
cancer has spread to 4 to 9 axillary lymph nodes and cancer in at least one of the lymph nodes is larger than 2 millimeters. Cancer has also spread to lymph nodes near the breastbone on the same side of the body as the primary tumor, and the cancer is larger than 0.2 millimeters and is found by sentinel lymph node biopsy.
- N3c: cancer has spread to lymph nodes above the collarbone on the same side of the body as the primary tumor.
When the lymph nodes are checked using mammography or ultrasound, it is called clinical staging. The clinical staging of lymph nodes is not described here.
Metastasis (M). The spread of cancer to other parts of the body.
- M0: There is no sign that cancer has spread to other parts of the body.
- M1: Cancer has spread to other parts of the body, most often the bones, lungs, liver, or brain. If cancer has spread to distant lymph nodes, the cancer in the lymph nodes is larger than 0.2 millimeters. The cancer is called metastatic breast cancer.
The grading system is used to describe how quickly a breast tumor is likely to grow and spread.
The grading system describes a tumor based on how abnormal the cancer cells and tissue look under a microscope and how quickly the cancer cells are likely to grow and spread. Low-grade cancer cells look more like normal cells and tend to grow and spread more slowly than high-grade cancer cells. To describe how abnormal the cancer cells and tissue are, the pathologist will assess the following three features:
- How much of the tumor tissue has normal breast ducts.
- The size and shape of the nuclei in the tumor cells.
- How many dividing cells are present, which is a measure of how fast the tumor cells are growing and dividing.
For each feature, the pathologist assigns a score of 1 to 3; a score of "1" means the cells and tumor tissue look the most like normal cells and tissue, and a score of "3" means the cells and tissue look the most abnormal. The scores for each feature are added together to get a total score between 3 and 9.
Three grades are possible:
- Total score of 3 to 5: G1 (Low grade or well differentiated).
- Total score of 6 to 7: G2 (Intermediate grade or moderately differentiated).
- Total score of 8 to 9: G3 (High grade or poorly differentiated).
Biomarker testing is used to find out whether breast cancer cells have certain receptors.
Healthy breast cells, and some breast cancer cells, have receptors (biomarkers) that attach to the hormones estrogen and progesterone. These hormones are needed for healthy cells, and some breast cancer cells, to grow and divide. To check for these biomarkers, samples of tissue containing breast cancer cells are removed during a biopsy or surgery. The samples are tested in a laboratory to see whether the breast cancer cells have estrogen or progesterone receptors.
Another type of receptor (biomarker) that is found on the surface of all breast cancer cells is called HER2. HER2 receptors are needed for the breast cancer cells to grow and divide.
For breast cancer, biomarker testing includes the following:
- Estrogen receptor (ER). If the breast cancer cells have estrogen receptors, the cancer cells are called ER positive (ER+). If the breast cancer cells do not have estrogen receptors, the cancer cells are called ER negative (ER-).
- Progesterone receptor (PR). If the breast cancer cells have progesterone receptors, the cancer cells are called PR positive (PR+). If the breast cancer cells do not have progesterone receptors, the cancer cells are called PR negative (PR-).
- Human epidermal growth factor type 2 receptor (HER2/neu or HER2). If the breast cancer cells have larger than normal amounts of HER2 receptors on their surface, the cancer cells are called HER2 positive (HER2+). If the breast cancer cells have a normal amount of HER2 on their surface, the cancer cells are called HER2 negative (HER2-). HER2+ breast cancer is more likely to grow and divide faster than HER2- breast cancer.
Sometimes the breast cancer cells will be described as triple negative or triple positive.
- Triple negative. If the breast cancer cells do not have estrogen receptors, progesterone receptors, or a larger than normal amount of HER2 receptors, the cancer cells are called triple negative.
- Triple positive. If the breast cancer cells do have estrogen receptors, progesterone receptors, and a larger than normal amount of HER2 receptors, the cancer cells are called triple positive.
It is important to know the estrogen receptor, progesterone receptor, and HER2 receptor status to choose the best treatment. There are drugs that can stop the receptors from attaching to the hormones estrogen and progesterone and stop the cancer from growing. Other drugs may be used to block the HER2 receptors on the surface of the breast cancer cells and stop the cancer from growing.
The TNM system, the grading system, and biomarker status are combined to find out the breast cancer stage.
Here are 3 examples that combine the TNM system, the grading system, and the biomarker status to find out the Pathological Prognostic breast cancer stage for a woman whose first treatment was surgery:
If the tumor size is 30 millimeters (T2), has not spread to nearby lymph nodes (N0), has not spread to distant parts of the body (M0), and is:
- Grade 1
- HER2+
- ER-
- PR-
The cancer is stage IIA.
If the tumor size is 53 millimeters (T3), has spread to 4 to 9 axillary lymph nodes (N2), has not spread to other parts of the body (M0), and is:
- Grade 2
- HER2+
- ER+
- PR-
The tumor is stage IIIA.
If the tumor size is 65 millimeters (T3), has spread to 3 axillary lymph nodes (N1a), has spread to the lungs (M1), and is:
- Grade 1
- HER2+
- ER-
- PR-
The cancer is stage IV (metastatic breast cancer).
Talk to your doctor to find out what your breast cancer stage is and how it is used to plan the best treatment for you.
After surgery, your doctor will receive a pathology report that describes the size and location of the primary tumor, the spread of cancer to nearby lymph nodes, tumor grade, and whether certain biomarkers are present. The pathology report and other test results are used to determine your breast cancer stage.
You are likely to have many questions. Ask your doctor to explain how staging is used to decide the best options to treat your cancer and whether there are clinical trials that might be right for you.
Treatment Option Overview
Treatment options for pregnant women depend on the stage of the disease and the trimester of the pregnancy.
Three types of standard treatment are used:
Surgery
Most pregnant women with breast cancer have surgery to remove the breast. Some of the lymph nodes under the arm may be removed so they can be checked under a microscope by a pathologist for signs of cancer.
Types of surgery to remove the cancer include:
- Modified radical mastectomy: Surgery to remove the whole breast that has cancer. This may include removal of the nipple, areola (the dark-colored skin around the nipple), and skin over the breast. Most of the lymph nodes under the arm are also removed.
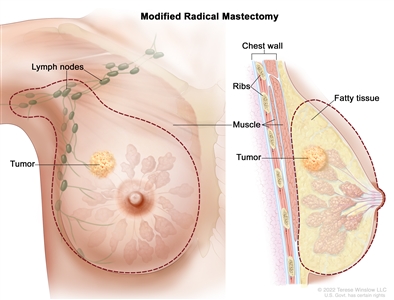
Modified radical mastectomy. The whole breast and most of the lymph nodes under the arm are removed. - Breast-conserving surgery: Surgery to remove the cancer and some normal tissue around it, but not the breast itself. Part of the chest wall lining may also be removed if the cancer is near it. This type of surgery may also be called lumpectomy, partial mastectomy, segmental mastectomy, quadrantectomy, or breast-sparing surgery.
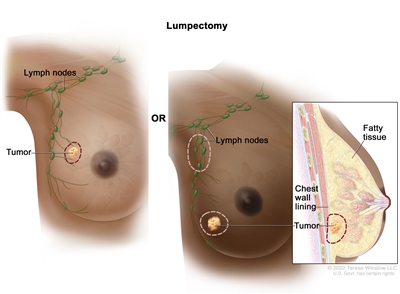
Lumpectomy. The tumor and some normal tissue around it are removed, but not the breast itself. Some lymph nodes under the arm may also be removed. If the cancer is near the chest wall, part of the chest wall lining may be removed as well.
After the doctor removes all of the cancer that can be seen at the time of surgery, some patients may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left. For pregnant women with early-stage breast cancer, radiation therapy and hormone therapy are given after the baby is born. Treatment given after surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer.
External radiation therapy may be given to pregnant women with early stage (stage I or II) breast cancer after the baby is born. Women with late stage (stage III or IV) breast cancer may be given external radiation therapy after the first 3 months of pregnancy or, if possible, radiation therapy is delayed until after the baby is born.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping the cells from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy).
Chemotherapy is usually not given during the first 3 months of pregnancy. Chemotherapy given after this time does not usually harm the fetus but may cause early labor or low birth weight.
See Drugs Approved for Breast Cancer for more information.
Ending the pregnancy does not seem to improve the mother's chance of survival.
Because ending the pregnancy is not likely to improve the mother's chance of survival, it is not usually a treatment option.
Treatment for breast cancer may cause side effects.
For information about side effects caused by treatment for cancer, visit our Side Effects page.
Treatment of Early Stage Breast Cancer During Pregnancy
For information about the treatments listed below, see the Treatment Option Overview section.
Pregnant women with early-stage breast cancer (stage I and stage II) are usually treated in the same way as patients who are not pregnant, with some changes to protect the fetus. Treatment may include the following:
- Modified radical mastectomy, if the breast cancer was diagnosed early in pregnancy.
- Breast-conserving surgery, if the breast cancer is diagnosed later in pregnancy. Radiation therapy may be given after the baby is born.
- Modified radical mastectomy or breast-conserving surgery during pregnancy. After the first 3 months of pregnancy, certain types of chemotherapy may be given before or after surgery.
Hormone therapy and trastuzumab should not be given during pregnancy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Late-Stage Breast Cancer During Pregnancy
For information about the treatments listed below, see the Treatment Option Overview section.
There is no standard treatment for patients with late-stage breast cancer (stage III or stage IV) during pregnancy. Treatment may include the following:
- Radiation therapy.
- Chemotherapy.
Radiation therapy and chemotherapy should not be given during the first 3 months of pregnancy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Special Issues About Breast Cancer During Pregnancy
Lactation (breast milk production) and breast-feeding should be stopped if surgery or chemotherapy is planned.
If surgery is planned, breast-feeding should be stopped to reduce blood flow in the breasts and make them smaller. Many chemotherapy drugs, especially cyclophosphamide and methotrexate, may occur in high levels in breast milk and may harm the nursing baby. Women receiving chemotherapy should not breast-feed.
Stopping lactation does not improve the mother's prognosis.
Breast cancer does not appear to harm the fetus.
Breast cancer cells do not seem to pass from the mother to the fetus.
Pregnancy does not seem to affect the survival of women who have had breast cancer in the past.
For women who have had breast cancer, pregnancy does not seem to affect their survival. However, some doctors recommend that a woman wait 2 years after treatment for breast cancer before trying to have a baby, so that any early return of the cancer would be detected. This may affect a woman's decision to become pregnant.
To Learn More About Breast Cancer During Pregnancy
For more information from the National Cancer Institute about breast cancer during pregnancy, see the following:
- Breast Cancer Home Page
- Breast Cancer Prevention
- Breast Cancer Screening
- Surgery Choices for Women with DCIS or Breast Cancer
- Dense Breasts: Answers to Commonly Asked Questions
- Drugs Approved for Breast Cancer
For general cancer information and other resources from the National Cancer Institute, visit:
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of breast cancer during pregnancy. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Adult Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Breast Cancer Treatment During Pregnancy. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/breast/patient/pregnancy-breast-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389161]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2022-12-14
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.

