Benign Prostatic Hyperplasia (BPH)
Condition Basics
What is benign prostatic hyperplasia (BPH)?
Benign prostatic hyperplasia (BPH) is an enlarged prostate gland. The prostate gland surrounds the urethra, the tube that carries urine from the bladder out of the body. As the prostate gets bigger, it may squeeze or partly block the urethra. This often causes problems with urinating.
BPH occurs in almost all men as they age. It is a common problem in older men. BPH is not cancer. But an enlarged prostate can cause urinary symptoms that need treatment.
What causes it?
BPH is probably a normal part of aging in men, caused by changes in hormones and cell growth. Genetics may play a role, especially for severe BPH in men younger than 60. Men older than 50 have higher chances of developing BPH. Experts don't know why some men have more severe symptoms than others.
What are the symptoms?
BPH causes urinary problems such as trouble starting and stopping the flow of urine, needing to urinate often, or feeling like your bladder isn't completely empty after you urinate. BPH does not cause prostate cancer and does not affect a man's ability to father children. It does not cause erection problems.
How is it diagnosed?
Your doctor can diagnose BPH by asking about your symptoms and health and by doing a physical exam. Tests may include a urine test and a digital rectal exam. This lets your doctor feel the size of your prostate. Sometimes a prostate-specific antigen (PSA) test is done to help rule out prostate cancer.
How is BPH treated?
In most cases, you don't need treatment unless symptoms bother you or you have problems such as backed-up urine, bladder infections, or bladder stones. Medicines may help reduce symptoms. Home treatment, such as avoiding alcohol, may also help. Sometimes surgery is done to remove part of your prostate.
Symptoms
BPH causes urinary problems such as:
- Having trouble getting a urine stream started and completely stopped (dribbling).
- Often feeling like you need to urinate. This feeling may even wake you up at night.
- Having a weak urine stream.
- Having a sense that your bladder is not completely empty after you urinate.
Many men with BPH have no symptoms.
In a small number of cases, BPH may cause the bladder to be blocked. This makes it impossible or extremely hard to urinate. This problem may cause backed-up urine (urinary retention), leading to bladder infections, bladder stones, or kidney damage.
What Happens
Every man's experience with BPH is different. Symptoms may get worse over time. For example, BPH can cause problems with urinating. In rare cases, severe obstruction of the urine flow can lead to complications. The complications can include complete or partial blockage of the urethra, or a urinary tract infection (UTI).
Learn more
When to Call
Call your doctor now if:
- You can't urinate at all.
- Urination is painful and you have a fever, chills, or body aches.
- You have pain in your lower back, just below your rib cage (flank pain), that is not related to an injury or physical effort.
- There is blood or pus in your urine or semen.
Call your doctor if you have painful urination and any of the following signs of a possible urinary tract infection or prostate infection that last longer than 24 hours:
- A burning sensation while urinating
- Painful ejaculation
- Problems controlling your urination during the day or at night
Call your doctor if you have urination problems that have developed over a few weeks or a few months and that happen often.
Watchful waiting
If urinary symptoms are minor or they don't bother you too much, and you don't have prostate cancer or a prostate infection, it may be okay to try watchful waiting or home treatment. Call a doctor if your symptoms change or get worse or if you change your mind about treatment.
Check your symptoms
Exams and Tests
Your doctor can diagnose BPH by asking about your symptoms and past health and by doing a physical exam. Your doctor may ask you how often you have symptoms of BPH, how severe they are, and how much they affect your life.
Tests may include a urine test (urinalysis) and a digital rectal exam. The exam lets your doctor feel the size of your prostate. In some cases, a prostate-specific antigen (PSA) test is done to help rule out prostate cancer. (Prostate cancer and BPH are not related, but they can cause some of the same symptoms.)
Your doctor may do other tests to check things such as your kidney and bladder function.
Learn more
Treatment Overview
In most cases, you don't need treatment for BPH unless the symptoms bother you or you have problems such as backed-up urine, bladder infections, or bladder stones.
Home treatment can help reduce or control your symptoms. It includes avoiding caffeine, alcohol, and medicines that make it hard to urinate.
If home treatment doesn't help, BPH can be treated with medicine. It can reduce the symptoms, but it rarely gets rid of them. If you stop taking the medicine, symptoms return.
If you have complications such as not being able to urinate, or your symptoms don't get better with medicines, your doctor may recommend surgery.
Self-Care
The following tips may make it easier to deal with your benign prostatic hyperplasia (BPH) symptoms.
- Practice "double voiding."
Urinate as much as possible, relax for a few moments, and then urinate again.
- Try sitting on the toilet instead of standing.
Or, after urinating while standing, sit on the toilet and try to urinate a little more.
- If you often wake up because you need to urinate, limit your fluid intake in the evening. And empty your bladder before bedtime.
- Avoid alcohol and caffeine.
They can make your body try to get rid of water and can make you urinate more often.
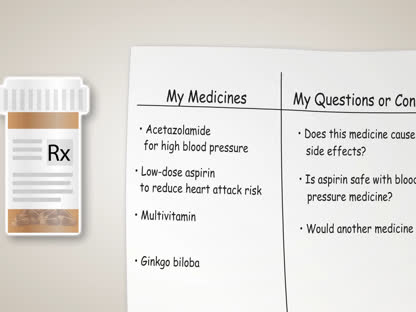
- If possible, avoid medicines that can make it difficult to urinate, such as nonprescription antihistamines, decongestants (including nasal sprays), and allergy pills.
Check with your doctor or pharmacist about all of the medicines you take.
Medicines
Medicines are sometimes used to help relieve BPH symptoms. If you stop using medicine, symptoms usually come back.
Medicines include:
- Alpha-blockers. They relieve symptoms within a few weeks. But they don't stop the process of prostate enlargement. They include tamsulosin (Flomax) and terazosin (Hytrin).
- 5-alpha reductase inhibitors. These may reduce the size of an enlarged prostate. They may take 6 months or more to show any effect on symptoms. They include dutasteride (Avodart) and finasteride (Proscar).
- Anticholinergic agents. They may help with urinary problems related to an overactive bladder, such as frequency, urgency, or incontinence. They include tolterodine (Detrol) and oxybutynin (Ditropan).
- Phosphodiesterase-5 (PDE-5) inhibitors. These may reduce BPH symptoms for men who also have erectile dysfunction. An example is tadalafil (Cialis).
Combining medicines, such as an alpha-blocker with a 5-alpha reductase inhibitor, may improve symptoms more than either medicine alone.
The side effects will vary based on the medicine.
Watch
Surgery
Surgery is done to decrease urinary symptoms and improve urine flow. Most surgeries do this by removing prostate tissue that is pressing on the urethra.
You may need surgery for BPH if you:
- Can't urinate.
- Have a partial blockage in your urethra.
- Keep having blood in your urine.
- Have kidney damage.
Your options for surgery will depend on many things, like the size of your prostate, your symptoms, concerns about complications, and your surgeon's experience.
Surgery often greatly improves the quality of life for those with severe symptoms. But surgery may cause erection problems or ejaculation problems. It may also make it hard to control urination (urinary incontinence).
Surgery choices
Types of surgery include:
- Transurethral resection of the prostate (TURP).
- Transurethral vaporization of the prostate (TUVP).
- Laser therapies.
- Thermal ablation therapies.
- Transurethral incision of the prostate (TUIP).
- Prostatic urethral lift (PUL), also called UroLift.
- Simple prostatectomy.
Learn more
Credits
Current as of: April 30, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: April 30, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.