
At first glance, stroke statistics offer some encouragement. Although this is still a leading cause of death and disability, fewer older Americans are having strokes, and death rates overall are declining.
But look deeper and some disturbing trends become clear:
- African Americans are 50 percent more likely to have a stroke than their white counterparts, and they are 70 percent more likely to die.
- Strokes kill more women than men, and 1 in 5 women will have a stroke. The risk is even higher for African American women.
- Since 2013, as stroke death rates declined among all races and ethnicities, however, Latinos have experienced a continued increase in fatal strokes. Stroke is the third leading cause of death for Latina women.
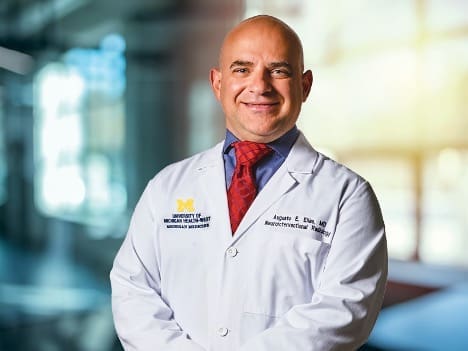
Dr. Augusto Elias sees these disparities first-hand in his role as medical director for Neurointerventional and Comprehensive Stroke Services at University of Michigan Health-West. Because May is Stroke Awareness Month, it’s a good time to remind everyone – particularly vulnerable groups – of the risk factors, Elias said.
“As a Latino, this hits home,” he said. “What I am seeing when I treat stroke cases is that African American and Latino patients are coming in at a younger age, with more risk factors and less healthcare overall. For example, more African American women are arriving at the Emergency Department with hemorrhagic stroke who either had a prior history of rupture or with larger undiagnosed aneurysms, because they have not been receiving preventive care.”
Prevention is crucial
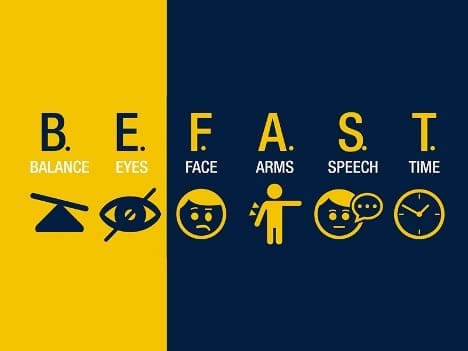
Thanks to education efforts like the B.E. F.A.S.T. campaign, more people across all populations are aware of the signs of stroke and the need for immediate medical help. But Elias said it’s even more important to recognize the risk factors to help prevent the stroke from happening in the first place.
He would like to see patients become advocates for themselves, as well as family members and friends, by being able to recognize the risk factors. For vulnerable groups especially, it’s important to reduce those risks that can be controlled by:
- Managing diabetes and high blood pressure
- Eating a sensible diet
- Getting exercise
- Stopping tobacco use
- Practicing moderation with alcohol
- Keeping regular visits with a primary care provider
“Take an active role and have that conversation with your doctor to reduce your overall risk,” Elias said. “This is an important message for those communities that have been cautious about seeking care.”
Making connections
Delivering that message requires overcoming skepticism stemming from the historic medical mistreatment of African Americans, as well as language barriers for other groups. Elias would also like to see more connections with the Native American community.
As an organization that values Diversity, Equity & Inclusion, UMH-West recently launched an Office of Health Equity to support ongoing efforts to address health disparities. This complements longstanding outreach programs, including bilingual education, to reach high-risk communities.
One way that UMH-West fosters engagement with diverse groups is through its Employee Resource Groups – forums for employees with common demographic characteristics and interests. These include groups for employees interested in supporting women, African Americans, Asian Americans, and LGBTQIA+ employees.
Elias is executive sponsor of the group called Mi Gente (Spanish for “My People”). Like the other ERGs, Mi Gente leverages the perspectives and voices of its members to support inclusion and promote community outreach.
“Through the leadership of (UMH-West CEO) Dr. Peter Hahn, there is a concerted effort to really actively participate, to support our entire community, and to create outreach programs,” Elias said. “My perspective now, with support from the top, is how we focus on specific disease processes – whether it’s cerebrovascular, cardiovascular, etc. – to make sure everyone accesses the care and prevention they need.”
Stroke disparities are not limited to race and ethnicity. Poverty often is a barrier to healthcare. Gender, including the higher risk for women, and gender identity also are factors.
Because LGBTQIA+ patients often have felt unwelcome or even been denied healthcare in the past, UMH-West has strengthened its efforts to provide a welcoming and inclusive environment. The health system recently gained national recognition for a commitment to equity and inclusion for lesbian, gay, bisexual, transgender and queer patients, families and employees.
“We’re heading the right way as an organization in order to address these disparities,” Elias said. “I believe it’s going to make a difference.”