Skin Cancer Prevention (PDQ®): Prevention - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
What is prevention?
Cancer prevention is action taken to lower the chance of getting cancer. By preventing cancer, the number of new cases of cancer in a group or population is lowered. Hopefully, this will lower the number of deaths caused by cancer.
To prevent new cancers from starting, scientists look at risk factors and protective factors. Anything that increases your chance of developing cancer is called a cancer risk factor; anything that decreases your chance of developing cancer is called a cancer protective factor.
Some risk factors for cancer can be avoided, but many cannot. For example, both smoking and inheriting certain genes are risk factors for some types of cancer, but only smoking can be avoided. Regular exercise and a healthy diet may be protective factors for some types of cancer. Avoiding risk factors and increasing protective factors may lower your risk but it does not mean that you will not get cancer.
Different ways to prevent cancer are being studied.
General Information About Skin Cancer
Skin cancer is a disease in which malignant (cancer) cells form in the tissues of the skin.
The skin is the body's largest organ. It protects against heat, sunlight, injury, and infection. Skin also helps control body temperature and stores water, fat, and vitamin D. The skin has several layers, but the two main layers are the epidermis (upper or outer layer) and the dermis (lower or inner layer).
The epidermis is made up of three kinds of cells:
- Squamous cells are the thin, flat cells that make up most of the epidermis.
- Basal cells are the round cells under the squamous cells.
- Melanocytes are found throughout the lower part of the epidermis. They make melanin, the pigment that gives skin its natural color. When skin is exposed to the sun, melanocytes make more pigment, causing the skin to tan, or darken.
The dermis contains blood and lymph vessels, hair follicles, and glands.
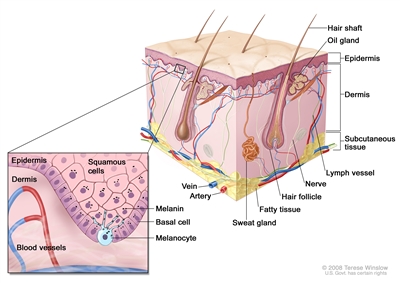
Anatomy of the skin, showing the epidermis, dermis, and subcutaneous tissue. Melanocytes are in the layer of basal cells at the deepest part of the epidermis.
For more information about skin cancer, see the following:
There are several types of skin cancer.
There are two main types of skin cancer:
- Nonmelanoma or keratinocyte carcinoma, which includes:
- Squamous cell carcinoma (SCC).
- Basal cell carcinoma.
- Melanoma.
The most common types of skin cancer are squamous cell carcinoma, which forms in the squamous cells, and basal cell carcinoma, which forms in the basal cells. Squamous cell carcinoma and basal cell carcinoma are also called keratinocyte carcinoma or nonmelanoma skin cancers. Melanoma, which forms in the melanocytes, is a less common type of skin cancer that grows and spreads quickly.
Skin cancer can occur anywhere on the body, but it is most common in areas exposed to sunlight, such as the face, neck, hands, and arms.
Skin cancer is the most common cancer in the United States.
Basal cell carcinoma and squamous cell carcinoma are the most common types of skin cancer in the United States. The number of new cases of nonmelanoma skin cancer appears to be increasing every year. These nonmelanoma skin cancers can usually be cured.
The number of new cases of melanoma has been increasing for at least 40 years. Melanoma is more likely to spread to nearby tissues and other parts of the body and can be harder to cure. Finding and treating melanoma skin cancer early may help prevent death from melanoma.
Skin Cancer Prevention
Avoiding risk factors and increasing protective factors may help prevent cancer.
Avoiding cancer risk factors may help prevent certain cancers. Risk factors include smoking, having overweight, and not getting enough exercise. Increasing protective factors such as quitting smoking and exercising may also help prevent some cancers. Talk to your doctor or other health care professional about how you might lower your risk of cancer.
Being exposed to ultraviolet radiation is a risk factor for skin cancer.
Some studies suggest that being exposed to ultraviolet (UV) radiation and the sensitivity of a person's skin to UV radiation are risk factors for skin cancer. UV radiation is the name for the invisible rays that are part of the energy that comes from the sun. Sunlamps and tanning beds also give off UV radiation.
Risk factors for nonmelanoma and melanoma cancers are not the same.
Risk factors for nonmelanoma skin cancer:
|
Risk factors for melanoma skin cancer:
|
Although having a fair complexion is a risk factor for nonmelanoma and melanoma skin cancer, people of all skin colors can get skin cancer.
Treatment of sun-damaged skin to prevent skin cancer:
Topical fluorouracil
A study showed that topical fluorouracil applied on sun-damaged skin daily for up to 4 weeks prevented new actinic keratoses from developing. The areas treated with topical fluorouracil had a lowered risk of developing into squamous cell carcinoma that would require surgery. The lowered risk of developing into squamous cell carcinoma was seen for 1 year after treatment. Topical fluorouracil did not, however, change the risk of developing basal cell carcinoma.
It is not known if the following lower the risk of nonmelanoma skin cancer:
Sunscreen use and avoiding sun exposure
It is not known if nonmelanoma skin cancer risk is decreased by staying out of the sun, using sunscreens, or wearing protective clothing when outdoors. This is because not enough studies have been done to prove this.
Sunscreen has been shown to prevent sunburns and actinic keratoses that may become squamous cell carcinoma, and to decrease the signs and symptoms of existing actinic keratoses.
The harms of using sunscreen are likely to be small and include allergic reactions to skin creams and lower levels of vitamin D made in the skin because of less sun exposure.
It is also possible that when a person uses sunscreen to avoid sunburn they may spend too much time in the sun and be exposed to harmful UV radiation.
Although protecting the skin and eyes from the sun has not been proven to lower the chance of getting skin cancer, skin experts suggest the following:
- Use sunscreen that protects against UV radiation.
- Do not stay out in the sun for long periods of time, especially when the sun is at its strongest.
- Wear long sleeve shirts, long pants, sun hats, and sunglasses, when outdoors.
Chemopreventive agents
Chemoprevention is the use of drugs, vitamins, or other agents to try to reduce the risk of cancer. The following chemopreventive agents have been studied to find whether they lower the risk of nonmelanoma skin cancer:
Beta carotene
Studies of beta carotene (taken as a supplement in pills) have not shown that it prevents nonmelanoma skin cancer from forming or coming back.
Isotretinoin and related retinoids
Retinoids are Vitamin A or vitamin A-like compounds that are applied to the skin or taken by mouth. Isotretinoin is a type of retinoid being studied in the prevention and treatment of certain cancers.
High doses of isotretinoin taken by mouth have been shown to prevent new skin cancers in patients with xeroderma pigmentosum. Isotretinoin cream has not been shown to prevent nonmelanoma skin cancers from coming back in patients previously treated for nonmelanoma skin cancers. These treatments can cause serious side effects.
Selenium
Studies have shown that selenium (taken in brewer's yeast tablets) does not lower the risk of basal cell carcinoma, and may increase the risk of squamous cell carcinoma.
Celecoxib
A study of celecoxib, a nonsteroidal anti-inflammatory drug (NSAID), in patients with actinic keratosis and a history of nonmelanoma skin cancer found those who took celecoxib had slightly lower rates of recurrent nonmelanoma skin cancers. Celecoxib may cause serious heart and blood vessel side effects.
Alpha-difluoromethylornithine (DFMO)
A study of alpha-difluoromethylornithine (DFMO) in patients with a history of nonmelanoma skin cancer showed that those who took DFMO had lower rates of basal cell carcinomas than those who took a placebo, but no difference in squamous cell carcinoma rates. However, those who took DFMO had greater hearing loss than the placebo group, leading to a higher rate of patients discontinuing this drug.
Nicotinamide (vitamin B3)
Studies have shown that nicotinamide (vitamin B3) helps prevent new actinic keratoses lesions from forming in people who had four or fewer actinic lesions before taking nicotinamide. However, one study also showed an increased incidence of nonmelanoma skin cancers in patients months after they were treated with nicotinamide. More studies are needed to find out if nicotinamide prevents nonmelanoma skin cancer from forming or coming back.
It is not known if the following lower the risk of melanoma:
Sunscreen
It has not been proven that using sunscreen to prevent sunburn can protect against melanoma caused by UV radiation. Other risk factors such as having skin that burns easily, having many benign (noncancerous) moles, or having atypical nevi may also play a role in whether melanoma forms.
Counseling and protecting the skin from the sun
Studies show that people who receive counseling or information about avoiding sun exposure improve their sun protective habits. These studies show mixed effects on reducing sunburns and do not show whether skin cancers are reduced.
Harms of avoiding sun exposure may include mood disorders, sleep disturbances, higher blood pressure, and impaired vitamin D metabolism..
Cancer prevention clinical trials are used to study ways to prevent cancer.
Cancer prevention clinical trials are used to study ways to lower the risk of developing certain types of cancer. Some cancer prevention trials are conducted with healthy people who have not had cancer but who have an increased risk for cancer. Other prevention trials are conducted with people who have had cancer and are trying to prevent another cancer of the same type or to lower their chance of developing a new type of cancer. Other trials are done with healthy volunteers who are not known to have any risk factors for cancer.
The purpose of some cancer prevention clinical trials is to find out whether actions people take can prevent cancer. These may include eating fruits and vegetables, exercising, quitting smoking, or taking certain medicines, vitamins, minerals, or food supplements.
New ways to prevent skin cancer are being studied in clinical trials.
Information about clinical trials supported by NCI can be found on NCI's clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about skin cancer prevention. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Screening and Prevention Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Screening and Prevention Editorial Board. PDQ Skin Cancer Prevention. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/skin/patient/skin-prevention-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389434]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2023-10-23
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.

