Top of the pageCheck Your Symptoms
Respiratory Problems, Age 11 and Younger
Overview
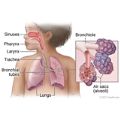
Most babies and older children have several mild infections of the respiratory system each year.
Upper respiratory system
The upper respiratory system includes the nose, mouth, sinuses, and throat. A child with an upper respiratory infection may feel uncomfortable and sound very congested. Other symptoms include:
- A runny or stuffy nose. It may lead to blocked nasal passages that cause the child to breathe through the mouth.
- Feeling cranky or restless, having a poor appetite, and being less active than usual.
- Coughing, especially when lying down.
- Fever.
Lower respiratory system
The lower respiratory system includes the bronchial tubes and lungs. These types of problems are less common than ones in the upper respiratory system. But they are usually more severe. They are more likely to need a doctor's care.
Symptoms of lower respiratory system infections include:
- Coughing that lasts through the day and night.
- Fever. It may be high with some infections, such as pneumonia.
- Feeling cranky or restless, having a poor appetite, and being less active than usual.
- Difficulty breathing. You may notice:
- Rapid breathing.
- Grunting, which is heard when the child breathes out (exhales). Most babies grunt now and then when they sleep. But grunting that occurs with rapid, shallow breathing may mean a lower respiratory system infection.
- Wheezing. (This is a different sound than croup.)
- Using the neck, chest, and belly muscles to breathe. This causes a "sucking in" between or under the ribs (retractions).
- Flaring the nostrils when breathing.
Respiratory problems may have many causes.
Viral infections
Viral infections cause most upper respiratory infections. Sore throats, colds, croup, and influenza (flu) are common viral illnesses in babies and older children. These infections are usually mild and go away in 4 to 10 days. But sometimes they can be severe.
Home treatment can help relieve the child's symptoms. The infection usually improves on its own within a week and is gone within 14 days.
Antibiotics aren't used to treat viral illnesses. They don't change the course of viral infections. Using an antibiotic when it's not needed exposes your child to the risks of an allergic reaction and antibiotic side effects. These side effects include nausea, vomiting, diarrhea, rashes, and yeast infections. Antibiotics also may kill helpful bacteria and encourage the growth of dangerous antibiotic-resistant bacteria.
Viral lower respiratory system infections may be mild, similar to upper respiratory system infections. An example of a possibly serious viral infection is bronchiolitis. Up to 10% of babies and children with viral infections of the lower respiratory system, such as those caused by respiratory syncytial virus (RSV), may have severe blockage of the air passages. They need treatment in a hospital.
Bacterial infections
The most common sites for bacterial infections in the upper respiratory system are the sinuses and throat.
Bacterial pneumonia may follow a viral illness as a secondary infection. Or it can appear as the first sign of a lower respiratory infection. In babies and small children, the first sign of infection often is rapid breathing, crankiness, being less active than usual, and poor feeding. Antibiotics work well against bacterial infections.
Allergies
Allergies are a common cause of respiratory problems. The symptoms in children include:
- Clear, runny drainage from the nose or a stuffy nose. Children often rub their noses by pushing the tip upward with the palm of the hand ("allergic salute").
- Sneezing and watery eyes. Often there are dark circles under the eyes ("allergic shiners").
- Crankiness and loss of appetite.
Asthma
Babies and small children usually don't have asthma. But the number of new cases of asthma increases with age.
- In babies and small children, a hacking cough may be the only symptom of mild asthma.
- If asthma gets worse, symptoms may include wheezing and shortness of breath after exercise or at nighttime.
- In severe asthma, the most common symptoms are trouble breathing (using the neck, chest, and belly muscles to breathe) and a high-pitched sound when breathing (wheezing).
- Allergies and asthma often occur together.
Other causes
Besides asthma, allergies, and infection, other possible causes of respiratory problems in children include:
- Exposure to cigarette smoke. Tobacco smoke impairs lung growth and development. Children who are exposed to this smoke, even before birth (prenatal), are more likely to have asthma and other respiratory problems.
- Blockage of the airway by an inhaled object, such as food, a piece of a balloon, or a small toy.
- Problems that have been present from birth (genetic causes), such as cystic fibrosis.
Babies and children younger than age 3 may have more symptoms with respiratory problems than older children. And they may become more ill. For this reason, younger children need to be watched more closely. What type of symptoms your child has and how severe they are will help you know if your child needs to see a doctor.
Check Your Symptoms
The medical assessment of symptoms is based on the body parts you have.
- If you are transgender or nonbinary, choose the sex that matches the body parts (such as ovaries, testes, prostate, breasts, penis, or vagina) you now have in the area where you are having symptoms.
- If your symptoms aren’t related to those organs, you can choose the gender you identify with.
- If you have some organs of both sexes, you may need to go through this triage tool twice (once as "male" and once as "female"). This will make sure that the tool asks the right questions for you.
Many things can affect how your body responds to a symptom and what kind of care you may need. These include:
- Your age. Babies and older adults tend to get sicker quicker.
- Your overall health. If you have a condition such as diabetes, HIV, cancer, or heart disease, you may need to pay closer attention to certain symptoms and seek care sooner.
- Medicines you take. Certain medicines, such as blood thinners (anticoagulants), medicines that suppress the immune system like steroids or chemotherapy, herbal remedies, or supplements can cause symptoms or make them worse.
- Recent health events, such as surgery or injury. These kinds of events can cause symptoms afterwards or make them more serious.
- Your health habits and lifestyle, such as eating and exercise habits, smoking, alcohol or drug use, sexual history, and travel.
Try Home Treatment
You have answered all the questions. Based on your answers, you may be able to take care of this problem at home.
- Try home treatment to relieve the symptoms.
- Call your doctor if symptoms get worse or you have any concerns (for example, if symptoms are not getting better as you would expect). You may need care sooner.
Symptoms of serious illness in a baby may include the following:
- The baby is limp and floppy like a rag doll.
- The baby doesn't respond at all to being held, touched, or talked to.
- The baby is hard to wake up.
Symptoms of serious illness may include:
- A severe headache.
- A stiff neck.
- Mental changes, such as feeling confused or much less alert.
- Extreme fatigue (to the point where it's hard for you to function).
- Shaking chills.
If you're not sure if a child's fever is high, moderate, or mild, think about these issues:
With a high fever:
- The child feels very hot.
- It is likely one of the highest fevers the child has ever had.
With a moderate fever:
- The child feels warm or hot.
- You are sure the child has a fever.
With a mild fever:
- The child may feel a little warm.
- You think the child might have a fever, but you're not sure.
Symptoms of difficulty breathing can range from mild to severe. For example:
- You may feel a little out of breath but still be able to talk (mild difficulty breathing), or you may be so out of breath that you cannot talk at all (severe difficulty breathing).
- It may be getting hard to breathe with activity (mild difficulty breathing), or you may have to work very hard to breathe even when you're at rest (severe difficulty breathing).
Symptoms of difficulty breathing in a baby or young child can range from mild to severe. For example:
- The child may be breathing a little faster than usual (mild difficulty breathing), or the child may be having so much trouble that the nostrils are flaring and the belly is moving in and out with every breath (severe difficulty breathing).
- The child may seem a little out of breath but is still able to eat or talk (mild difficulty breathing), or the child may be breathing so hard that he or she cannot eat or talk (severe difficulty breathing).
Severe trouble breathing means:
- The child cannot eat or talk because he or she is breathing so hard.
- The child's nostrils are flaring and the belly is moving in and out with every breath.
- The child seems to be tiring out.
- The child seems very sleepy or confused.
Moderate trouble breathing means:
- The child is breathing a lot faster than usual.
- The child has to take breaks from eating or talking to breathe.
- The nostrils flare or the belly moves in and out at times when the child breathes.
Mild trouble breathing means:
- The child is breathing a little faster than usual.
- The child seems a little out of breath but can still eat or talk.
A baby that is extremely sick:
- May be limp and floppy like a rag doll.
- May not respond at all to being held, touched, or talked to.
- May be hard to wake up.
A baby that is sick (but not extremely sick):
- May be sleepier than usual.
- May not eat or drink as much as usual.
Temperature varies a little depending on how you measure it. For children up to 11 years old, here are the ranges for high, moderate, and mild according to how you took the temperature.
Oral (by mouth), ear, or rectal temperature
- High: 104° F (40° C) and higher
- Moderate: 100.4° F (38° C) to 103.9° F (39.9° C)
- Mild: 100.3° F (37.9° C) and lower
A forehead (temporal) scanner is usually 0.5° F (0.3° C) to 1° F (0.6° C) lower than an oral temperature.
Armpit (axillary) temperature
- High: 103° F (39.5° C) and higher
- Moderate: 99.4° F (37.4° C) to 102.9° F (39.4° C)
- Mild: 99.3° F (37.3° C) and lower
Note: For children under 5 years old, rectal temperatures are the most accurate.
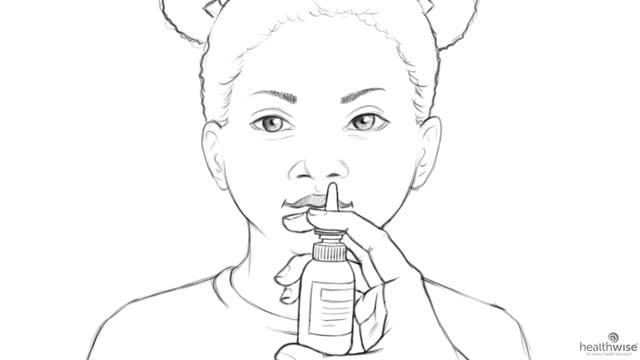
You can use a small rubber bulb (called an aspirating bulb) to remove mucus from your baby's nose or mouth when a cold or allergies make it hard for the baby to eat, sleep, or breathe.
To use the bulb:
- Put a few saline nose drops in each side of the baby's nose before you start.
- Position the baby with his or her head tilted slightly back.
- Squeeze the round base of the bulb.
- Gently insert the tip of the bulb tightly inside the baby's nose.
- Release the bulb to remove (suction) mucus from the nose.
Don't do this more than 5 or 6 times a day. Doing it too often can make the congestion worse and can also cause the lining of the nose to swell or bleed.
Certain health conditions and medicines weaken the immune system's ability to fight off infection and illness. Some examples in children are:
- Diseases such as diabetes, cystic fibrosis, sickle cell disease, and congenital heart disease.
- Steroid medicines, which are used to treat a variety of conditions.
- Medicines taken after organ transplant.
- Chemotherapy and radiation therapy for cancer.
- Not having a spleen.
Sudden drooling and trouble swallowing can be signs of a serious problem called epiglottitis. This problem can happen at any age.
The epiglottis is a flap of tissue at the back of the throat that you can't see when you look in the mouth. When you swallow, it closes to keep food and fluids out of the tube (trachea) that leads to the lungs. If the epiglottis becomes inflamed or infected, it can swell and quickly block the airway. This makes it very hard to breathe.
The symptoms start suddenly. A person with epiglottitis is likely to seem very sick, have a fever, drool, and have trouble breathing, swallowing, and making sounds. In the case of a child, you may notice the child trying to sit up and lean forward with his or her jaw forward, because it's easier to breathe in this position.
Seek Care Now
Based on your answers, you may need care right away. The problem is likely to get worse without medical care.
- Call your doctor now to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or you don't have one, seek care in the next hour.
- You do not need to call an ambulance unless:
- You cannot travel safely either by driving yourself or by having someone else drive you.
- You are in an area where heavy traffic or other problems may slow you down.
Call 911 Now
Based on your answers, you need emergency care.
Call 911 or other emergency services now.
Sometimes people don't want to call 911. They may think that their symptoms aren't serious or that they can just get someone else to drive them. Or they might be concerned about the cost. But based on your answers, the safest and quickest way for you to get the care you need is to call 911 for medical transport to the hospital.
Seek Care Today
Based on your answers, you may need care soon. The problem probably will not get better without medical care.
- Call your doctor or telehealth provider today to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or telehealth provider or you don't have one, seek care today.
- If it is evening, watch the symptoms and seek care in the morning.
- If the symptoms get worse, seek care sooner.
What are your options for medical care?
Today your options for where to get your medical care are greater than ever before. You may not even have to leave your home to get the care you want and need. You can choose based on what your health problem is and what works best for you.
- Telehealth is a video call with a health care provider. It can be a convenient way to get medical advice or treatment. Some insurers provide access to telehealth that may be available 24 hours a day. Telehealth for less serious problems may cost less and be faster than in-person clinic visits.
- Urgent care and retail clinics are options if you don't have a doctor, you can't or don't want to wait to see your own doctor, or a telehealth visit can’t treat the problem.
- Virtual care from your primary provider or a telehealth service can be delivered through your smartphone, computer, or tablet.
Make an Appointment
Based on your answers, the problem may not improve without medical care.
- Make an appointment to see your doctor in the next 1 to 2 weeks, or contact your telehealth provider.
- If appropriate, try home treatment while you are waiting for the appointment.
- If symptoms get worse or you have any concerns, call your doctor or telehealth provider. You may need care sooner.
What are your options for medical care?
Today your options for where to get your medical care are greater than ever before. You may not even have to leave your home to get the care you want and need. You can choose based on what your health problem is and what works best for you.
- Telehealth is a video call with a health care provider. It can be a convenient way to get medical advice or treatment. Some insurers provide access to telehealth that may be available 24 hours a day. Telehealth for less serious problems may cost less and be faster than in-person clinic visits.
- Urgent care and retail clinics are options if you don't have a doctor, you can't or don't want to wait to see your own doctor, or a telehealth visit can’t treat the problem.
- Virtual care from your primary provider or a telehealth service can be delivered through your smartphone, computer, or tablet.
Self-Care
Most children have 7 to 10 mild upper respiratory infections each year. Your child may feel uncomfortable and have a stuffy nose. The infection is usually better within a week and is usually gone within 14 days.
Here are some things you can do to ease mild symptoms and help your child feel better.
- Be safe with medicines. Read and follow all instructions on the label.
- Ask your doctor if you can give your child acetaminophen (Tylenol) or ibuprofen (Advil, Motrin). Do not use ibuprofen if your child is less than 6 months old unless the doctor gave you instructions to use it.
- Do not give aspirin to anyone younger than 20. It has been linked to Reye syndrome, a serious illness.
- Be careful with cough and cold medicines. Don't give them to children younger than 6, because they don't work for children that age and can even be harmful. For children 6 and older, always follow all the instructions carefully. Make sure you know how much medicine to give and how long to use it. And use the dosing device if one is included.
- Be careful when giving your child over-the-counter cold or flu medicines and Tylenol at the same time. Many of these medicines have acetaminophen, which is Tylenol. Read the labels to make sure that you are not giving your child more than the recommended dose. Too much acetaminophen (Tylenol) can be harmful.
- Don't give your child leftover antibiotics. And don't give your child antibiotics or other medicines prescribed for someone else.
- Have your child drink plenty of water and other fluids.
This may help soothe a dry or sore throat. Honey or lemon juice in hot water or tea may ease a dry cough. Do not give honey to a child younger than 1 year old. It may contain bacteria that are harmful to infants.
- Try moist air.
Place a cool-mist humidifier by your child's bed or close to your child. This may make it easier for your child to breathe. Follow the directions for cleaning the machine.
- Treat a stuffy nose.
- If your child has problems breathing because of a stuffy nose, squirt a few saline (saltwater) nasal drops in one nostril. Then have your child blow their nose. Repeat for the other nostril. Do not do this more than 5 or 6 times a day.
- For babies and children who aren't able to blow their nose, put a few saline drops in one nostril. Using a soft rubber suction bulb, squeeze air out of the bulb and gently place the tip of the bulb inside the baby's nose. Relax your hand to suck the mucus from the nose. Repeat in the other nostril.
- Make sure your child rests.
Keep your child at home if they have a fever.
- Keep your child away from smoke.
Do not smoke or let anyone else smoke around your child or in your home.
Using decongestants
Here are some precautions to take when using decongestants.
- Be safe with medicines. Read and follow all instructions on the label.
- Decongestants may not be safe for young children. The U.S. Food and Drug Administration (FDA) recommends not using over-the-counter cough and cold medicines in children younger than age 2. The FDA also recommends avoiding these medicines for children younger than age 4.footnote 1 If you use these medicines, always follow the directions about how much to use based on age and in some cases weight. Not everyone needs the same amount of medicine.
- Decongestants can cause problems for people who have certain health problems, such as heart disease, high blood pressure, glaucoma, diabetes, or an overactive thyroid. Decongestants may also interact with some drugs, such as certain antidepressants and high blood pressure medicines. Read the package carefully or ask your pharmacist or doctor to help you choose the best decongestant for you.
- Drink extra fluids when you are taking cold and allergy medicines.
- Don't use decongestant nasal sprays, drops, or gels more times in one day or for more days in a row than the label says. Overuse can cause rebound congestion. It makes your mucous membranes swell up more than before you used the spray.
- If you are pregnant or breastfeeding, check with your doctor or pharmacist before using a decongestant.
When to call for help during self-care
Call a doctor if any of the following occur during self-care at home:
- New or worse trouble breathing.
- New wheezing.
- New or worse cough.
- Symptoms occur more often or are more severe.
Learn more
Watch
Preparing For Your Appointment
You can help your doctor diagnose and treat your condition by being prepared for your appointment.
Credits
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.